Subscribe to The Model Health Show:
TMHS 487: The Rise In Infectious Diseases, Autoimmunity, & The Gut-Immune Connection – With Dr. Emeran Mayer
Every year, we learn more about the role and function of the gut microbiome. Our microbiome plays a tremendous role in our overall health including regulating our immune system, body composition, and so much more. But even with our ever-expanding understanding of the microbiome, our modern-day habits and practices are failing to support our gut health.
On this episode of The Model Health Show, our guest is Dr. Emeran Mayer. Dr. Mayer is a world-renowned gastroenterologist and neuroscientist, one of the world’s most foremost experts on the gut-brain connection, and the author of the new groundbreaking book, The Gut-Immune Connection. On today’s show, he’s sharing incredible insights from his work on gut microbes, human immune health, and how optimizing your microbiome can impact your state of health.
You’re going to hear Dr. Mayer’s work on the link between the microbiome and common Western diseases and how our compromised microbiomes are making us more susceptible to viruses. This episode also contains conversations on food quality and policy, antibiotic use, and real-world tips you can implement to support the health of your microbiome. Enjoy!
In this episode you’ll discover:
- What percentage of immune cells exist in the gut.
- How gut microbes work.
- Why your gut is technically your first brain.
- How the digestive system evolved over time.
- The two basic design principles that have been maintained in evolution.
- How many genes microbes have.
- What happens to microbes during mass extinction.
- How microbial signals can affect health and disease.
- The hidden cost of chemicals in agriculture.
- How treating the soil impacts the nutrient content of our food.
- What regenerative organic agriculture is, and why it’s important.
- How the corporatization of our food system has hurt our health.
- What it means to have a richness and diversity of microbes.
- Why we need to focus on gut health to prevent the next pandemic.
- What comorbidities actually are.
- Why food quality is a sociological and political issue.
- The hidden danger of antibiotic overuse.
- How our microbiomes are damaged from birth.
- What you need to know about antibiotic levels in animal products.
- How autoimmune diseases are triggered.
- Why microbes are so adaptive, and how they compare to human immune cells.
- How fear and stress impact the immune system.
- Why exposure to pets is beneficial for the microbiome.
- What you need to know about taking supplements for immune health.
- The pros and cons of intermittent fasting.
- How sleep cycles impact immune health.
- What the One Health Concept is.
Items mentioned in this episode include:
- PaleoValley.com/model — Use code MODEL for 15% off!
- Organifi.com/Model — Use the coupon code MODEL for 20% off!
- The Gut-Immune Connection by Dr. Emeran Mayer
- The Mind-Gut Connection by Dr. Emeran Mayer
- Missing Microbes by Dr. Martin J. Blaser
- CNN: Cash-Strapped Farmers Feed Candy to Cows
- Connect with Dr. Emeran Mayer Website / Facebook / Twitter / Instagram
Thank you so much for checking out this episode of The Model Health Show. If you haven’t done so already, please take a minute and leave a quick rating and review of the show on Apple Podcast by clicking on the link below. It will help us to keep delivering life-changing information for you every week!
Transcript:
SHAWN STEVENSON: Welcome to The Model Health Show. This is fitness and nutrition expert, Shawn Stevenson, and I'm so grateful for you tune in with me today. We are at an incredible crossroads with our health and human civilization. Right now, we're dealing with an infectious disease that has gone viral. It has gone viral, it's a virus that has gone viral. There are many aspects of this equation that are being overlooked right now, and so today we're going to dive in. We're going to to talk with one of the foremost experts in the world on immune system function, and I want to highlight this by saying, for example, we're talking about in the context of COVID-19. It's a viral infection that is a tropism towards our lung tissue. So, it's targeting our lung tissue, it's where some of this hyper-activity of the immune system, the inflammation, the degradation of the capillaries involving the lungs. All these things are taking place, but what's not talked about is the fact that we have a microbiome of our lungs that are really an interface interacting with the microbes that we're exposed to, the viruses we're exposed to, the pathogenic bacteria we're exposed to.
We have a microbiome within our lungs, that is a regulatory force in all of this. What are we doing to support the microbiome of our lungs? What are we doing to support the hub of our microbiome itself? The hub of our immune system itself, which as you're going to learn today, from somebody who's been in this field as a gastroenterologist, studying this for 40 years. It's become common knowledge today, the importance of the microbiome, but he's one of the originators and one of the pioneers in the field, helping to educate the public and students as he is working with students at UCLA in understanding the importance of this dynamic in the hub of our immune system. About 70% of our immune system is located within our gastrointestinal tract, within our gut, this is how important this is. This interaction with our microbiome and the integrity of our gut itself is one of the most important fundamental things that we need to address right now, because our immune system is under fire, our immune system, not from viruses per se, but from our environmental conditions, creating the susceptibility and the degradation of our immune system, allowing these things to really take us down.
And so, the question is, "What are we going to do about it?" So that's what we're going to dive into today. We're going to address and really break this down and look at how all these systems work, and what are some of the intelligent steps that we can take to fortify and to make us more resilient moving forward? So really pumped about that and obviously, our nutrition is a foundational piece in this. It's feeding our microbes the things that are advantageous, because it's really our gut microbes who are interacting with our food first, they're the front line deciding what's going to get shuttled into our tissues, for example. What are they going to nibble on? And what is going to get into our, "human cells"? And we know that key nutrients, for example, are hallmarks of immune system integrity and immune system function. One that everybody knows, every man, woman and child knows is vitamin C. But the question is how? Why does vitamin C work? Why is it important? Well, vitamin C is a regulatory force, it has roles that it's playing specifically in regeneration of tissues, so helping to heal damage but not just that, but also just general growth and not just repair, but growth and development of our tissues and cells. So, Vitamin C has a big role in repair, and as far as the defense side, do we have any clinical evidence regarding COVID-19 and vitamin C?
Well, check this out, a recent study cited in the journal, Pharma Nutrition, investigated the impact of vitamin C in relation to the cytokine activity associated with COVID-19. So, this is the cytokine storm that has been the headline and on the tip of a lot of people's tongues in regards to COVID-19, and what they found is that vitamin C is effective at inhibiting the production of cytokine storms. These should be headlines, but early on, unfortunately, in all of these things taking place, this information was not only put on a lower tier of importance, some of it was even blocked. It was censored, you weren't able to talk about foundational principles regarding immune system, so key nutrients. But for me, I'm still looking at this with a more balanced perspective, because I don't want folks haphazardly running out and getting some synthetic form of vitamin C, when in reality we need to get educated about what does vitamin C really do? And also, what are the most advantageous sources? What are the most bile available sources? What are the sources of vitamin C that have bile potentiators to make it work effectively in the body and not just be wasted on us in a sense, and not bile available, not absorbable?
And what imbalances come along if we're just dumping massive amounts of supplemental synthetic vitamin C in our bodies without the other co-factors that keep it in balance? So, these are all questions that we're being presented with an opportunity to understand a little bit better. And so, for me, this is why I'm such a huge advocate of botanical, super concentrated, high vitamin C dense foods like camu camu berry, C-A-M-U C-A-M-U. I've been a fan, been studying, been utilizing camu camu berry for over 15 years, it's one of my all-time favorite things. And the big reason is that just under a teaspoon of camu camu berry powder provides about 700% of your RDA in vitamin C, but it really does show up as a powerful protection for our tissues, unlike isolated vitamin C products. This is highlighted in a study published in the Journal of Cardiology. And it had folks who are proactively creating damage and oxidation of their tissues, it had 20 male smokers to consume camu camu berry daily over the course of a one-week study period. And what happened was, the camu camu berry consumption led to significantly lowered oxidative stress and reduced inflammatory biomarkers like C-reactive protein.
So, these are things that we're seeing with infectious diseases as well, damaging the lungs. And what's more, here's the thing, there were no changes in these markers in the placebo group, who received an ordinary vitamin C tablet, an ordinary synthetic version of vitamin C. The camu camu berry did something special. And for that, the research has indicated that the combination of other antioxidants from the camu camu berries had a more powerful antioxidant effect than standard vitamin C products alone. Camu camu berry, number one. Number two, amla berry. Amla berry. Again, been studying for years, one of my favorite things. Acerola cherry, these are three of the most concentrated sources of vitamin C ever discovered, and massive amounts of peer-reviewed evidence as to their efficacy. And they're all combined contained in a formula I'm so grateful for, that there's a formula that actually has all three. I used to buy them separately. I'd get it from this company, that company, but now there's one that has all three without any binders, fillers, unnecessary ingredients that comes along with so many different supplements today. They might even get an organic version of a super food, and then there's coming along with binders and fillers, and chemical additives that a lot of folks don't realize the detrimental effects of those things.
The essential C-formula from Paleovalley, is in a league of its own, period. This is something you need to have in your cabinet. In your super food cabinet. The vitamin C concentration is remarkable, but it's all of the other bio-potentiators and co-factors, the other antioxidants found within these super foods that makes it so special. Head over to PaleoValley.com/model. That's P-A-L-E-O-V-A-L-L-E-Y.COM/model. Again, PaleoValley.com/model, use the code model, you get 15% off their essential c-formula, and their turmeric complex is out of this world as well. So, so good, they've got incredible snacks for the family, all grown and prepared the right way, really paying attention to regenerative agriculture. This company is just incredible. Check them out, PaleoValley.com/model. Now, let's get to the Apple Podcast review of the week.
ITUNES REVIEW: Another five-star review titled “Fantastic Podcast” by AuntJenny5. “I just found this podcast in the last six or so months, I'm sorry I did not find it much sooner, I love the content and format as well as the study-based information that Shawn provides, the content is interesting and relevant. Thank you for your hard work and an amazing podcast”.
SHAWN STEVENSON: Wow, thank you for leaving that review over on Apple Podcast, I appreciate it so much. And listen, if you've yet to do so, pop over to Apple Podcast and leave a review for the Model Health Show. I appreciate it immensely. And on that note, let's get to our special guest and topic of the day. Renowned gastroenterologist and neuroscientist, Dr. Emeran Mayer is one of the world's foremost experts on the gut-brain connection. Over the past 40 years, his research and published work has offered ground-breaking evidence of the critical role of bio-directional interaction between the brain and the gut. And more recently, on the role of the gut microbiome in these interactions. With implications not only for gastrointestinal diseases, but for metabolic, emotional and cognitive health. And this was long before the topic of the microbiome became a buzzword or something that's very popular in our lexicon, in the world of health and wellness today. And now in his new book, The Gut-Immune Connection: How Understanding Why We're Sick Can Help Us Regain Our Health, Dr. Mayer proposes a radical paradigm shift, in which he puts the gut microbiome and the gut-based immune system at the center of our current health epidemics. Let's jump into this conversation with the incredible Dr. Emeran Mayer. Well, first of all, Dr. Mayer, thank you so much for joining us on the show today.
DR. EMERAN MAYER: Well, thanks for having me on the show, Shawn.
SHAWN STEVENSON: It's my pleasure, it's my pleasure. So, I'm so grateful to talk to you because you've been in this field for four decades now, and now a lot of the stuff that you've been learning and teaching, and really working to get to the public, to get to students, now it's becoming a part of our lexicon in understanding the connection, for example, between our microbiome, our gut, and our immune system. So, can we start with that, can you share some insights about how our gut, our microbiome, and our immune system are really interconnected?
DR. EMERAN MAYER: So, in a zooming internal GI tract, it's not just the tube that processes and transports food from the stomach into the intestine, and if you look into deeper with a microscope and dissecting it, you'll notice that it is a very complex organ. So, a few microns, you go inside the wall of the GI tract and you find the biggest part of our immune system, 70% of our immune cells are located in the gut, and you don't see it, they're silent. And they don't just sit there, but they also move throughout the body to other areas and send their signaling molecules, if that system is activated throughout the body. The microbes are separated only by... I mean again, this is all in the magnitude of microns, so less than a millimeter. So, the microbes are sitting just very close to that immune system location, they're only separated by two things. One is a mucus layer made out of sugar molecules, and the other one is the lining of the gut, these are cells that are very tightly connected to each other.
And they separate these 40 trillion microbes from our immune system, and it's kind of an amazing engineering feat that nature has produced there. Who would dare to put the most sensitive system in our body, the immune system, that senses everything that's foreign and potentially dangerous from 40 trillion microbes? They're all beneficial to us, the ones that live in our gut, but every once in a while, there's other microbes that you ingest or that get into your GI tract that could kill you. So that barrier is pretty one of the most important things, that barrier that separates the inside of the gut with its microbial world from the immune system, that barrier is the key to understanding what's a healthy gut and what happens if that barrier breaks down because that starts a whole avalanche of things that first localized in the gut, but then it goes throughout the body reaching all organs.
SHAWN STEVENSON: Yeah, that should be just really startling for us, first of all, that 70% of our immune system is located in our gut. And this interaction with all these 40 trillion microbes and how close proximity that it is, the influence that they have is obvious once you understand that. But you said in our design, and that makes me think about in your book, you mentioned how we often refer to the gut as the second brain, but it's really the first brain.
DR. EMERAN MAYER: It is the first brain. And so, in evolution, the first marine animals were called hydras, there are still descendants of these animals around today, they were basically a floating digestive tube, tiny, a few millimeters and they had a nerve net wrapped around them. And so, the first life formed was a very simple digestive tube, which ingested things in one end and expelled the residue on the other end, and this nerve net that was wrapped around this tube regulated the contractions and the expulsion of waste material. This is another amazing thing, that design from really billions of years ago has been maintained in pretty much all life forms. So, these cockroaches, snakes, fish have that design that you have, a nervous system wrapped around the gut. And what happened, at some point... So, this is like the enteric nervous system, and later from that developed in more complex animals, we need a central nervous system that doesn't just focus on the gut but focuses on the world around us.
And interestingly also that at some point in the ocean, as these things were floating around the ocean that probably by chance, some microbes that were the dominant life form in the ocean, ended up inside this digestive tube and started... This was a very beneficial thing for both because those microbes living in this floating gut essentially had free transportation where it was exposed to nutrients coming in and were protected. So, this was also maintained in evolution, so two basic design principles: A digestive system with a nervous system around it, and then inside with a microbial population that started to live in symbiosis with the other two systems. And yeah, it is kind of amazing. So, the molecules that the microbes brought with them because they have been living for 3.5 billion years in the oceans and had a lot of time to perfect their communication systems, and all the information that they... What they tested and what worked out, what didn't work out, was encoded in their genes, so now microbes have 100 times more genes than humans have. We have 20,000 genes, microbes have their genes number in the millions, and it's because they had a much, much longer than humans, time to collect this information.
And they transferred that information about how to build neurotransmitters, and single molecules to the nervous system in the gut and ultimately that information made it into our brain. So now, people always ask, "How could the microbes even communicate with something complex as the brain?" Well, it's because they use the same neurotransmitters and the same single molecules, and it came originally from the microbes, it's not that we gave the microbes our information how to design neurotransmitters, it's the other way around.
SHAWN STEVENSON: Yeah, that's so fascinating. So, we've got the enteric nervous system in the gut, enteroendocrine system in the gut, and that it's like a communication super highway in a sense. And I love this, as you talk about our reductionism transition in medicine where we just keep isolating everything when it's really so interconnected, and our development. We started off... Well, our vast, vast, long ago roots as just being a tube to extract nutrients, and we eventually sprouted... We had this, the gut being the first brain and then we sprouted another brain to handle other things basically. And we see that that's the final frontier. But really, our gut and the gut health, it's all coming back to that. And so, what I want to ask you about, in the same vein, you mentioned this really important thing, which is the genes. And I think that when they did the Human Genome Project, for example, we thought we would have like a million genes, for example, it's just 20,000. But we have such diversity in who we are, and I think a big part of that is the microbial diversity we carry within us. So, can you talk a little bit about that, comparing how many genes we have as humans to the genes that we might carry within our bodies that are microbial?
DR. EMERAN MAYER: Yeah, so this is a really important point, because initially people got excited to say 99% of our cells are not human, so just talking about the cells because that's how the science started, are not human, and they're bacterial. In the meantime, we know it's about 60-40% of the ratio, so almost a half-human and half were microbial, but if you go to the genetic level, then you realize that difference is much, much bigger. So, from 20,000 to 40-100 million genes in the microbes. And genes, basically, the gene number means information to build things and encode functions. Most of the functions of these genes, we don't really know.
SHAWN STEVENSON: Right.
DR. EMERAN MAYER: So, we're just scraping at the surface of this. But I think the biggest excitement, and if somebody goes into this field is, what are we going to find out what all this information does? And what role does it play in things you have never thought about are related to our genes, like brain function and aging? And so, there's going to be a lot of these unknown factors, but that I think it gives us the greatest... I sort of come to this point, if you say the genetic information somehow relates to the intelligence of that system, not the individual organism, they don't really have intelligence. If you think about a beehive or an anthill that has a certain intelligence as a collective thing. So, I think the microbiome, not just in the gut, but also there's communications with the microbiome in the soil and in the oceans, if you take that system together as one, look at it as one, and it's obviously spatially distributed like nothing else, and it's invisible on top of it.
SHAWN STEVENSON: Yeah.
DR. EMERAN MAYER: That's got to be the most intelligent system on the planet. And what that implies... I mean one thing that we can see with mass extinction, so we had five of those in evolution that most large animals disappeared, they could not survive these, the microbes didn't. The microbes survived all of this, so they have skills, and knowledge, and survival information stored of how to survive these dramatic climate changes and atmospheric changes. So, to me, that's one of the most exciting things that there's something inside of us that we don't see, we can't touch. So, you really have to use your imagination to think what goes on in there, but even if you go inside with an endoscope, you don't see it. But that invisible entity that lives in darkness, and without oxygen, it contributes this amazing amount of information to our health and plays a role if it's altered in our disease states.
SHAWN STEVENSON: That's remarkable. So, if we go gene for gene, at least 99% of our genes are microbial?
DR. EMERAN MAYER: Yes, yeah. Yeah, and so when I give my talks, I always show this figure, is a schematic figure. It's a white outline of a human being. And it's all white, and it's all microbial genetic information, and has a very thin lining in red which are the human genes, so it gives you an idea, which is like, yeah, it's this relationship, this dimension, is something awe-inspiring.
SHAWN STEVENSON: That's powerful. So, if we're understanding what genes are, which essentially they're instructions, and if we take that one tenet and understand that 99% of the genetic material that we're carrying around for go gene for gene is microbial, and understanding that they're inherently doing something, these genes or the microbes are inherently doing something, there's obviously going to be a big impact on all of the systems of our bodies. And I love this about your book because you talk about some of the various roles that our gut plays in diseases that affect different organs, like the brain, for example. So, can we talk about that a little bit?
DR. EMERAN MAYER: Yeah, so coming back to this interface in our gut between the micro-immune system, the endocrine system in the gut, so the largest part of the endocrine or hormonal system is also there. And that that interaction influences what immune system, what the hormone do that circulates through our body. Nothing stays in the gut. Some people say it's not Vagus. It doesn't stay in the gut.
SHAWN STEVENSON: Yeah.
DR. EMERAN MAYER: And so, these are all long-distance signaling mechanisms, and they...
SHAWN STEVENSON: And by the way, the Vagus nerve is there as well, for us to study.
DR. EMERAN MAYER: Yeah, the Vagus nerve is there. So, there's these different communication channels that amplify the signal, what happens in the gut, so if you want an example, you ingest something that the microbes have never seen in evolution, like a...
SHAWN STEVENSON: A Twinkie.
DR. EMERAN MAYER: So yeah, just... Or a pesticide.
SHAWN STEVENSON: Oh yeah.
DR. EMERAN MAYER: Roundup is a good example, they've never seen all of our medications, so the microbes with their knowledge, they can break this molecule down, they have enzymes that can break this down, they don't say, "Well, I've never seen this so I'm not... " So they break it down into smaller molecules that then interact with the immune system, or with the endocrine system, and then that generates the signal that goes through the body, and depending on your genetic vulnerability, so be it for Alzheimer's disease or be it for depression. When these signals get to the brain, they change the brain in a way that you have now a higher risk of developing these diseases. These microbial signals are not the only cause of these diseases, but in a vulnerable individual, they can trigger the transition from health into disease, and so this long distance signaling is clearly, so it can go through what we call neuro-active metabolites. So many things like the amino acid tryptophan microbes can break it down into other molecules that interact with the nervous system, some go into to the brain, some are turned into serotonin, this ubiquitous signaling molecule, so this is one way that they generate from our food substances that then are distributed through the body and to all the organs.
Another one is to the Vagus nerve, so the Vagus nerve has 90% of that nerve that connects all our organs with the brain, goes from the organ to the brain, so we still don't know what information is all transported in such a nerve. So, if something happens at the gut level, a microbe produces like short-chain fatty acids from breaking down fiber molecules, then acts on a receptor on the Vagus nerve and that goes to the brain. And the third one is the cell wall of the microbes itself is a signaling trigger. So, there's components like lipopolysaccharide or LPS. When that comes into contact with the receptor on an immune cell, it will trigger the activation of this immune cell which then produces cytokines, and these cytokines again goes throughout the body. So at least three parallel communication systems are engaged, which amplify and spread the message throughout the body, and if you use this network terminology, the gut is really the hub in this network, in this global mind-body network, anything that happens at the gut level has a high propensity to influence everything else.
SHAWN STEVENSON: Yeah, and again that should seem obvious at this point, and you being a pioneer in helping to bring this data to the public and seeing it, it start to really sprout and show, but you just mentioned that interaction with tryptophan, getting converted into serotonin, which is a precursor for melatonin, and we tend to think like sleep is a head thing, and a lot of it's rooted in the gut. The big focus, we have a hyper-focus when we're talking about anxiety and depression around certain neurotransmitters, which a lot of this is rooted in the gut, and yet a lot of attention isn't going to addressing the real root, and I got to mention this. Actually, when you mentioned the pesticide, it's so funny because I wrote this down earlier, and I didn't know if I was going to talk about this, but I was reviewing a study, and this was published in scientific reports, and it revealed that pesticides create a pro-inflammatory state in the gut, and here's the big thing, and why I wrote it down is that it was found to also disrupt microbial gene expression. Can you talk about the impact that industrial agriculture has had on our gut health? Because this is something you address in the book, and it's a really big deal.
DR. EMERAN MAYER: Yeah, this is a big thing. So industrial agriculture essentially is chemical agriculture, it's gone from an organic agriculture that is indigenous people use that way with natural fertilizers from the farm animals that go back into the ground. So, what modern agriculture has done particularly were increased in the last 75 years since World War II, to increase productivity and output and feeding the world, and that actually has been successful, but at a very high cost, because putting all these chemicals not just into the soil has killed a lot of the microbes. So similar what we have done with antibiotics in humans has a good side, wonderful side, but at the same time has a hidden cost that we now realize. The second thing is by killing a lot of the microbial ecosystems in the soil, the plants have lost the ability to produce their own medicine, which is a group of molecules called polyphenols, and that's a whole topic for, we could talk about this for an hour, it's one of my favorite topics.
That the soil microbes stimulate the plant roots to produce these molecules that then are transported up to the stem of the plant, into their leaves, into their fruit and defend them against any kind of stress, so it could be chemical stress, it could be insecticides, it could be drought anything that stresses the plant, generates a signal down into the root system, to communicate with the microbes in the soil, which then stimulates this medicine production, these phytochemicals, and in industrial agriculture that's greatly diminished.
SHAWN STEVENSON: Right.
DR. EMERAN MAYER: So that results in the need for pesticides and insecticides, because these plants are no longer... They grow like crazy, as long as you kill everything else around it.
SHAWN STEVENSON: Right, they're not adaptable.
DR. EMERAN MAYER: So, they're not adaptable, and so you start out with killing the microbes in the soil, then you have to start killing all the bugs, and the pests that could compromise this plant because it's no longer producing its own medicine. And so that's created this viscous cycle that they were now producing plants that look beautiful, you go to Gelson's or Whole Foods Market, and you see it is beautiful looking, but the nutrient content is not the same. 'Cause these molecules that protect the plant, at the same time are the main components of the nutrients that are contained in the plants, and when we eat these plants, a big health benefit, it's not just the fiber, but it's also these plant medicine molecules which...
SHAWN STEVENSON: Like polyphenols.
DR. EMERAN MAYER: Like polyphenols. So, we're now eating a diet that's really greatly diminished in this. And so, industrial agriculture, I like to call it chemical agriculture, has really played a major role. And then we're kind of coming back to realize that now there are some pioneers that promote this regenerative organic agriculture. Regenerative means you put things back into the soil, you don't just constantly extract things from it, but you put it back so the microbes can grow, and you restore that ecosystem. So, the people behind that kiss the ground, the Kiss the Ground movie, it's a good example. Yvon Chouinard from Patagonia is another example, who's really been pushing this concept. So, Ryland Engelhart is the mind behind the Kiss the Ground group and the movie. So, there's a growing number of people, and they have a plan to really change agriculture back into a regenerative organic system, which would solve a lot of problems. Because one of the things also... So, we don't really know what some of these pesticides and insecticides do to the plant, and then to our own... Because we eat the plants, to our own microbial ecosystem.
DR. EMERAN MAYER: Just for Glyphosate to get FDA approval, they only had to do a few studies, short-term studies in cultures of cells, and they found in human cells, and they found that glyphosate exposure to the substance that is a roundup, the glyphosate exposure did not really affect human cells, because human cells don't have that shikimate pathway to metabolize it. So, they concluded from a few short-term studies, it's safe, it doesn't affect human cells.
SHAWN STEVENSON: This is fine.
DR. EMERAN MAYER: This is way before the microbiome science came around. So, in the meantime we know microbes can break down most chemicals that we ingest, including glyphosate, and believe or not, there's very little science on that. And I don't know, it almost seems like... I hate to be a conspiracy theorist but it's almost like if that science is not supported, that you won't get funded doing this, 'cause the commercial interest and the lobby behind that industry is so gigantic that... I don't know, I don't want to get into any sort of political implications with this, but there's certainly... It's very surprising that at a time where we're so conscious of the health, the gut health and everything, that there's not a flurry of studies that show definitively that Glyphosate does harm, not just to our microbiome, but also secondarily, our own health.
SHAWN STEVENSON: Yeah, the regulatory systems are really backwards, because we're trying to prove that they're hurting us instead of proving that they're not hurting us.
DR. EMERAN MAYER: Yeah, yeah.
SHAWN STEVENSON: It's really backwards, and it should be obvious. Again, these are newly invented compounds. With the EPA, for example, there's close to 40,000 chemicals approved for use in fertilizers, it's so many. It's insane. And once we get in this conversation, so I mentioned earlier about directly damaging microbial gene expression, but that's just one part of it. Because, the ingestion of these chemicals can disrupt our microbiome, but also the lack of key nutrients, even if we're eating organic, the foods that we're eating today are lacking on these nutrients that feed our microbes. And so, this is what I want to ask you about next, because we've seen a direct impact, and you highlight this in the book, and it's so important, the direct impact is a vastly declining richness and diversity of our microbes. So, can you talk about those two different things? And the current state of our microbes versus people who are eating more of a normal diet.
DR. EMERAN MAYER: Yeah, so just to explain these two terms, and they are important. So that applies to any ecosystem, so the riches and diversity applies is not just for the microbiome. So, diversity means, how many different species of organisms are there? So high diversity would be something, if you extrapolate this to a city. If you have one couple from Latin America, and one couple from African-American, and one couple from Asia, and the rest is all Caucasian, so that's a diverse ecosystem because we have four different and it could be more diverse. But it's not necessarily a healthy ecosystem because that one representation of one species is not sufficient, you need a richness, so you need... If you did divide up the population, you would want to have 25% of each of these populations populating that ecosystem, and that's the richness. So, you need the richness, and the diversity in order to get... So, the main property then of such an ecosystem is, it's resilient against perturbations. Anything you do to it, it will bounce back, something will break down and it will be resistant to change. And that's clearly a property of our own microbiome.
It's a good and a bad thing. The good thing is, if you eat something, you get a giant infection, or you eat something bad, or have a stomach flu, it doesn't knock out your system, it always comes back on the system. Same with if you take an antibiotic once, it doesn't knock out your system, even though you kill or suppress all the organisms, it comes back because of its resistance or resilience to perturbation. The bad thing is, if you want to restore a sick microbiome like we do in... 'cause there's a lot of attempts now with this fecal microbial transplant, because we can do this in mice, artificial models, that you take a rich, diverse, and a healthy microbiome and put this into a mouse gut, you can do all kinds of things. You can make obese mouse lean, you can make a depressed mouse, a normal behavior. But you can only do this because these mice start out, these laboratory mice, without having any microbes, and there's so-called germ-free mice. So, in a situation like that, yes, you can change it if you put some in, but even in people that have a compromised microbiome, it's still resilient, so it won't allow you to do that.
There's very few conditions, there's actually literally just one condition where a fecal microbial transplant in humans has really worked, and that's because again, the resilience and the resistance for change. Our microbial... This ecosystem has been declining in both diversity and richness, so we are losing... And that just kind of perpetuated through generation, it gets worse, a little bit worse in each generation. We've been losing a lot of this diversity and richness, and some strains have disappeared that you find in populations like hunter-gatherer remnants in the world. So, we've lost a lot of these species, not species as much, but strains, and this is continuing. If you don't change something dramatically in how we interact with the environment and with our food and with the chemicals we use, this will continue. And some people have predicted it will lead to massive pandemics because it makes us more, and more vulnerable to infections. It's interesting, so a book came out a few years before the pandemic, Missing Microbes by Martin Blaser, and in his last chapter he talks about this, the threat of pandemics. This is way before the actual pandemic we're in now. So, we got a taste of it, what can become even worse in the future, I think.
SHAWN STEVENSON: This is really getting to a place of something very visceral for us because we're seeing again, firsthand, what you can really see coming from a mile away and understanding that truly a big regulatory force of what we see as our immune system has so much to do with the health of our gut. And in the book, you also detail, again, there's a decline. And if you want to look at it like an analogy of a rainforest and this loss of species and how does that affect other species and the richness and diversity and we've been losing these strains, many have gone extinct, many are... They're on the endangered list. And so we still have an opportunity to turn these things around, but I sent this paper over to you and I knew that you had already seen it, but I wanted to ask you about this because you also mentioned with the richness, it really holds within its ability to bounce back when we have any kind of intrusions or anything, any abnormalities is the ability to bounce back.
And this recent paper was published in the journal Gut, and is titled, Gut microbiota composition reflects disease severity and dysfunctional immune responses in patients with COVID-19. The researchers uncovered that hospitalized COVID-19 patients consistently have lower levels of immunomodulatory bacteria coinciding with higher levels of inflammation, and you would think that this would be getting more attention, and what I noticed also with the study that jumped out afterwards, and even more so now talking with you, is that they noted that even after they, "cleared" the virus, their microbes didn't bounce back, it was still at that kind of decline state where they're missing microbes that are associated with robust immune function.
DR. EMERAN MAYER: Yeah, no, this is a very interesting point. It has not received... I mean, this will receive a lot more attention, I'm sure. There's so much research going on in this field that in the next five years, we'll see papers coming out on many aspects but...
SHAWN STEVENSON: We needed yesterday though.
DR. EMERAN MAYER: Yeah, yeah. So, we've been so absorbed with fighting the pandemic and the vaccine development, which is phenomenal from a scientific standpoint, less so from preventing the next one and the next one will come. If you see, we've had several smaller ones. But with all the things going on that we've talked about before, the likelihood of these events is increasing. So, yeah, what is the connections? COVID-19 enters our body really through the respiratory system, so you're wondering what does the gut have to do with it? But then we talked earlier also about the fact that 70% of the immune system is in the gut. And a lot of the programming and modulation of the immune system that then goes to all the other organs happens at the gut level. So, then microbes have a big word to say on that. And so, the finding that they reported there could be interpreted in two ways. One is, if you have a compromised gut microbial system, that by itself will increase the risk that we have exaggerated immune responses to any perturbation.
And so, it's quite possible that these people that they studied they had these abnormalities before they got infected. In this study they brought in people that were infected and studied them, but in a real longitudinal study, you would want to know, and these studies are coming out. Somebody who didn't have it and then developed it, did they have this microbial abnormality before that put them in an increased risk? And I would say that's more likely because you also know... So, some people got a more severe form of the infection. Some developed this long COVID phenomenon that the symptoms don't go away, and people that are at a higher risk of developing these more severe forms are... So, we know who these high-risk populations are, unfortunately, it breaks down along socio-economic categories with socio-economic, even racial, and it's very not genetic. It's probably the correlation of socio-economic with racial...
SHAWN STEVENSON: Environment.
DR. EMERAN MAYER: Yeah, the environment. So that a big part of our population eats very unhealthy food either because it's cheaper, or because they don't have access to the whole food markets and all these healthy things that are being promoted. Like on the west side of LA, it's not... You go to downtown areas you don't see the same. So those segments of the population had the much higher risk of not just getting it but getting a more severe form and also for this long COVID complication. And we know people that are on this poor diet have a compromised microbial ecosystem, and they're missing exactly those organisms that they found in these patients. So, I think there's a pretty good link between... It's not just a biological thing, it's also sociological, it's a political thing, and hopefully will draw more attention to populations that were most severely affected. And in the jargon of the discussion in the media, it's always said with the people that have more comorbidities that are more likely to develop a more severe form. Well, what these comorbidities are, as I point out in my book, are the consequence of an unhealthy gut microbiome and over reactive immune system, so it all fits together. And I think regardless where this infection attacks your body, it will always be influenced by your gut health and indirectly then by the things that you feed your gut, your microbes.
SHAWN STEVENSON: Yeah. There's so much here, and I want to ask you about one of the common treatments that was being used for COVID very early on that you mentioned in the book, and how this might have contributed to exacerbating the problem even more, especially down the line. And we're going to talk about that right after this important break, you sit tight we'll be right back.
Researchers at Yale University School of Medicine, the research found that one of the biggest culprits behind our obesity epidemic is neuroinflammation. Brain inflammation increases the propensity of obesity and obesity increases the propensity, the likelihood of neuroinflammation, they go hand in hand. So, we've got to address this. One of the things that's been proven to help to reduce neuroinflammation is cited in a study published in PLOS One, Public Library of Science One, revealed that the super green algae Spirulina has the potential to one, improve neurogenesis in the brain. So the creation of new brain cells, specifically the hippocampus is where we get a lot. And the hippocampus is the memory center of the brain. This is kind of important. And two, the study revealed that Spirulina is able to directly reduce neuroinflammation, it's incredible. It's helping the structural integrity of this master gland, this master organ controlling everything about us. The most complicated object in the known universe is also one of the most fragile, we've gotta protect it. This is why for myself and my family, Spirulina, Chlorella, Ashwagandha, all of these powerful foods are put together in the incredible blend at Organifi.
This is a regular staple here in my family for good reason. Spirulina, in being one of the highlighted ingredients, not only does it have this benefit for neurogenesis and neuroinflammation but also has rare nutrients like phycocyanin, the same thing with Chlorella as well. That phycocyanin is one of the few things that can trigger stem cell genesis, the creation of new stem cells, very few things have been found to do that, and then Chlorella in the formula as well. And that growth factor, the Chlorella growth factor, it's just remarkable, and also its benefits in helping your body to metabolize and eliminate heavy metals, and the list goes on and on, it's incredible. But the bottomline is this; it tastes good, it tastes good. I have experimented for at least about 15 years at all these different green formulas, these different green superfood plants. Many of them is not very good. Okay, many of them, they shall remain nameless, but I've tried them back in the day before, tasting good was an option to just like, just get it in by any means necessary, if you gotta do the whole pinch the nose and get it done, whatever.
But now, pleasure leads to longevity, pleasure leads to taking a practice on it and imbibing it and making it part of your routine, your habits, your daily life, so this is why I appreciate the fact they've created a formula that actually tastes good, all organic. Cold process, so you actually retain and get the nutrients that we're looking for in Organifi, so pop over there, check it out, it's organifi.com/model, that's O-R-G-A-N-I-F-I.com/model and you get 20% off, 20% off their green juice formula, their red juice formula, and also their gold as well, so they've got some incredible blends, all done the right way, with integrity, again, organic, low temperature processed and yummy. Organifi, you got that yummy yummy, organifi.com/model and now back to the show.
Alright, and we're back and we're talking with Dr. Mayer about his new book that I've got right here, "The Gut Immune Connection", it is available right now. Go and pick up a copy, like yesterday, it is an important part of your library. Before the break, we were talking about the connection with our microbes and COVID, which is showing itself more and more in the data, and I'm so grateful for this too, as you mentioned. We've got great researchers out there who are asking these questions and looking into this, but if this would have even happened 20 years ago, this might not have been on many people's minds, except yours, and so seeing that this is unfolding, but in the book, you also mentioned that early on, a significant number of folks coming in with COVID, were being treated with antibiotics, so can you talk about that intersection with our declining richness and diversity in microbes and our rampant use and often overuse and often inappropriate use of antibiotics, when in this case, we were even dealing with a viral infection.
DR. EMERAN MAYER: Yeah, and again, coming back to this book, Missing Microbes by Martin Blaser. He put this, I mean, this is his main area of research, and in the meantime, a lot of people have picked up on that idea that we overuse antibiotics, dramatically. Antibiotics are the most important medical invention I would say that have saved millions, hundreds of millions of lives, but when it's used indiscriminately and without proper indications, it has a huge collateral damage on primarily on this microbial world, and it's in different ways. It starts at the time of delivery. So, prophylactic administration of antibiotics to women during delivery to prevent potential serious streptococcal infections is the first last of this microbial, I would call it poison to the emerging microbiome in the infant, then a lot of babies now are born prematurely, they end up in the Neonatal Intensive Care Unit, intensive exposure to antibiotics often for weeks to prevent infections, and then there's also the whole sterile environment during delivery that is typical for hospitals.
So, the exposure of the infant coming through the birth canal is also compromised, so we've done with antibiotics everything possible, even the first days of life to compromise that system. And it hasn't really changed dramatically, this has not changed, but then it goes on, if you look at the statistics of how many doses of antibiotics a two-year-old in the US is getting by the age of two, it's something between five and 10 doses of antibiotics, which is unbelievable. And then that increases over time. Part of the fault are overly concerned mothers, hypervigilant mothers, who think every time the kid has a severe respiratory tract infection that they need to get an antibiotic, and they go to their physician and many GPs or pediatricians will then give in and say, "Here's the prescription." And we know that viruses do not respond to antibiotics, so it's a complete ineffective treatment, which has this major effect, damaging effect on the evolving microbiome. This early phase is particularly important because the microbiome is programmed the first three years of life, the basic design, the basic ecosystem design is accomplished in the first three years, and so everything that you do during that time is particularly vulnerable, so most people invest in societies, going to this world with an antibiotic compromised microbiome system.
Defect later in life is not as traumatic, so there's studies, most people bounce back, and we come back to the resilience, from one dose of an antibiotic, a lot of people bounce back after three doses. But then depending on how stable your ecosystem is, some of them, some people will not bounce back, and they will then have... So, if as an adult, if you have a history of having received a lot of antibiotics as an infant, and now you get one or two or three courses of antibiotics, your microbiome will further be compromised. And we do this still today, a condition called irritable bowel syndrome, common condition, or IBS. So, one of the FDA-approved therapies is treatment with an antibiotic, which when you think about the implications of what I've just told you, it's the last thing you would want to do. Patients feel temporarily better with that antibiotic, but many of them, the symptoms come back, and then the response is, "Well, let's do another dose.
SHAWN STEVENSON: Yeah.
DR. EMERAN MAYER: And I've had patients who have had 10 doses of this antibiotic. So clinical medicine has not learned, in my opinion, enough from the insights that we have now about this damaging effect. It's not the only reason, I think that we see this progressively declining diversity and richness of the microbiome and the increase of diseases related to this, like autoimmune diseases or allergies. But it's definitely a big one, and which could easily be changed.
SHAWN STEVENSON: Yeah. As you mentioned, it's setting us up for more long-term problems, potentially. And you also mentioned that this was a game-changer in health, in having so many advantageous uses, but it's just kind of been transitioned into a place where it's a thing that we quickly jump to. And as you mentioned, from patients demanding it, to healthcare practitioners being a little bit overzealous or being very quick to pass out a prescription for antibiotic, when I think we've also gotten to a place where we are not used to just being sick as well, like of colds and flus and things of that nature, and allowing our bodies to recover. And I think that our bodies are also having a harder time recovering because of the loss of all these microbes. And I want to mention this too, because you mentioned the inoculation when we first come into the world, so that bathing and that kind of download in a sense, of our bacteria cascade, and plus making it a more and more sterile environment that we're living in, that our kids are living in.
And this is what I wanted to ask you about, which is in the book, you highlight something that should just jump right out at us, is the fact that our chronic diseases, not just infectious diseases, but chronic diseases are happening in younger and younger populations now, whether it's hypertension, heart disease, diabetes, obesity, the list goes on and on, and you make the connection between that and our microbes as well.
DR. EMERAN MAYER: Yeah, so this is one or of the more worrisome trends, and one particularly striking example to me is being a gastroenterologist, so the colon cancer screening guidelines that used to be at age 50, and then people have found... And this colon cancer screening has had beneficial effects of fewer people die from colon cancer, but what we noticed that now the onset of colon, or the first appearance of colon cancer has gone down to age 40, so now it's not a complication of people getting older, but it's really a younger population. Similar things have happened with diabetes, with autoimmune diseases, like inflammatory bowel disease. In all these seemingly unrelated diseases, we see this phenomenon that on the one side these diseases are starting, or exploding also in the developing world, not just in the developed world. But they're starting at young and younger age, which goes along with what we talked about, this onslaught, this massive attack, this warfare really, on microbes, that we don't perceive as warfare, we perceive it as treatments, but I think this mindset really has to change. And it's a combination, initially, particularly for the lay public, it's easier to say, "Okay, it's the antibiotics."
But in the meantime, we know it's these multiple things that are happening at the same time, it's the changes in the diet in the last 75 years which obviously also affect the microbes, it's the amount of chemicals, or what we call xenobiotics in science, that we expose our microbiome to. So all these things have been increasing. And what we see now on a macroscopic level, that we see these diseases coming early in life, say also whole market this people don't die as often from them, and the only reason is, it's not because these diseases are decreasing in their frequency, it's because we're throwing a massive amount of medications at this problem to suppress the immune system.
SHAWN STEVENSON: So, their process of dying is longer?
DR. EMERAN MAYER: Their process of dying is longer, it's not a healthy longevity, it's a longevity bought with the price of more and more medications that everybody automatically gets, like our statins for metabolic syndrome, for heart disease. So, our society has really responded to these changes that we now understand why they're happening, not with going to the root cause, but by throwing this, you know, from a scientific standpoint, it's phenomenal what these medications do, but it's not a solution to this problem, we can't continue like that. So, I think people who realize that... And one last thing about the antibiotics, we forgot one source, it's this exposure of our farm animals to antibiotics. So, we consume meat from animals that is soaked with antibiotics.
SHAWN STEVENSON: I believe 80% of the antibiotics used in our country is for the cattle.
DR. EMERAN MAYER: Yeah, yeah. So even if you think, "Yeah, so you've gone through a natural birth at home without the sterile hospital environment." If you eat the regular food supply, you'll still get your sufficient dose of antibiotics. And with animals, they're not even being used to... Well, they're being used to keep them from getting sick because of the unhealthy environment that we raise our farm animals, but also to simulate their growth, so for two reasons. For chickens, the same thing. In chickens, many, most diseases in chickens are viral, so we're doing the same mistake, we're throwing antibiotics at them. Well, we know that they don't do anything for these viral problems. Many examples in our food supply, shrimp farms, throwing tons of antibiotics into the shrimp farms, main diseases of shrimp are viral. Yeah, so it's a pretty sad state and it's going to take dramatic efforts to, on all levels, from the political lobbying, there is curtailing lobbying efforts to the aware consumer, that's ultimately where it ends up. So, if people don't buy the products, then there's not a market and then... So, I think what people like us can do, we can raise awareness.
SHAWN STEVENSON: I really want everybody to get this. You just said something one of the most mind-blowing things, which is, "Sure, we've got antibiotics in cattle feed to protect them against disease from the abnormal diets that they're being fed." The soy and all these things, even candy. There's practices where cows are being fed candy, for example, true, wrappers and all, we'll put the video for everybody in the show notes. But the main purpose of the antibiotics is to help them to gain weight faster, and I really want everybody to get this. Because you also touch on this in the book as well, the connection between the health of our microbiome and obesity and metabolic diseases and these things, again, that have skyrocketed. Changing that microbial cascade can make us better at assimilating calories, for example, better at adding weight to our frame. Not based on the diet, necessarily strictly alone, which is a big, huge part, and I want to talk more about that, but the change in our microbes can affect our body composition.
DR. EMERAN MAYER: Yeah, so this is interesting, that this phenomenon that veterinarians and the meat industry figured out a long time ago that you can actually... They didn't think about the gut microbes of the cows, that that played a role in it. But now we know that our gut microbial system plays a big role in obesity and particularly in metabolic syndrome, with the immune activation that goes along with that. That what benefited us on one side in industrial agriculture, turns out to be a major factor now in our healthcare crisis. I would say the obesity part is a big problem. Medically, it's more important the associated metabolic derangements that come with increased body weight and body mass index. So, it is shocking that again, we're adapting to this problem by... Now, it's no longer politically correct to... If you want to make a Facebook post and it has a picture of an obese person in it or mention the word obesity or overweight, then that's not politically correct and you may actually risk that it's taken down, and you notice in the news or in commercials, like all of a sudden, you used to have these slim actors in it, now all of a sudden, at least half of them are overweight. So, it's trying to normalize that phenomenon, which is crazy. I think people should much rather focus on, "What can I do not to go down this road of feeling okay if I am overweight?"
SHAWN STEVENSON: Yeah, because really what we're looking at is health, and I think that this is being reframed in a sense that it makes us... Instead of looking at the health implications like, "Hey, you're increasing all-cause mortality in your life for diabetes, for heart attacks for... " The list goes on and on, rapid increases in autoimmune conditions, neuro-degenerative conditions, the list goes on and on. And instead of us addressing the underlying issue, we're just normalizing things. And I love the fact in the book, because I haven't really seen this research in book form, much of anywhere else except in some of the books that I've written, coming out of the Weizmann Institute, you mentioned some of their data in your book as well. And they did this really fascinating study, they had folks across different time zones, and they've seen the change and shift in their cascade of bacteria, shifting to that, which looks more like that of a person who is overweight or obese. And so, they took those samples from these folks and implanted them, fecal samples, into lean mice. When they have this, quote, "Fat bacteria cascade"
And they also took bacteria samples from people who had a bacteria cascade associated with leanness and just, quote, "Normal" and then planted into lean mice. The lean mice who received that bacteria, nothing changed but the mice who received the fecal transplant from humans who had the bacteria shift to more of a cascade associated with obesity, these mice became insulin resistant. They gained weight and they gained body fat, not changing anything else about their diet, simply from changing their microbes. And so, I want people to really get the power of this in all aspects. And I want to circle back because this was one of the... I had to put the book down for a second and just sit with this after I read this statistic. One of the biggest issues we've seen recently in our culture is this skyrocketing incidence of autoimmune conditions. This used to be something that was pretty rare in our population, now it's become so normal. And the number, and I've never seen the number at first hand, about 50 million US citizens have an autoimmune condition now that they're struggling with. And so, can you talk about that aspect? Why are we seeing, which we already know the answer is such a rampant increase in autoimmune conditions and how does this play into kind of sorting out... And this is what I want to transition into, how can we address this? How can we fix this? The root and stop treating the symptoms?
DR. EMERAN MAYER: Yeah, so the autoimmune conditions, the story is a little bit different from these other metabolic conditions and these chronic non-infectious disease epidemic that we see in the heart and colon cancer and neurodegenerative diseases. This is something that starts, again, early in life. So not only do we program our gut microbiome early in life, but we also train our immune system early in life to differentiate between harmful and non-harmful influences and differentiating self and non-self. So, self normally is perceived as a beneficial or should be tolerated and non-self should be attacked. So, with all these things that we talked about earlier on, this increase in hygiene, being removed from farm animals, from dirt, from the soil, everything is being disinfected. So, this increases in hygiene and so they gave this whole area, this name, The Hygiene Hypothesis, that we're no longer exposed to things like even parasites. Like worms, which were very common in, probably 50, 70 years ago, and kids have a phase where they have worms. Also, organisms like H. Pylori, that plays a big role in ulcer disease which has lived with us for hundreds of thousands of years with humans. And all these organisms and the parasites that in a young age, if the immune system is exposed to these, they train the immune system that this is not something that needs to be killed.
So, this training phase requires influences from the environment. The exposures of non-lethal, but still foreign influences. And we've eliminated a lot of this. And this including the H. Pylori, almost eradicated completely. We don't know what the long-term effects of that is. And there were many benign forms of infections and infestations. So now the immune system in that infant grows up without lessons of how to differentiate between self and non-self, and good and bad, and...
SHAWN STEVENSON: So, this is our, also rapid increase in allergies?
DR. EMERAN MAYER: Exactly. So now we have this uneducated immune system that's hyper-reactive to a lot of things that should not trigger this immune response. And so, I was bringing up this example, that our microbes are rapidly adaptive, have this ability to rapidly adapt to new situations, including this new century of extreme hygiene and in eliminating many organisms that we think are harmful. But the human immune system doesn't have that rapid... None of the human cells have that rapid adaptability. They react in the way that they have been designed by our 20,000 genes in a way that if something doesn't make sense, they ring the alarm bell. So now you have this rapidly changing different microbiome system that interacts with a much more conservative and less reactive immune system. And that triggers the alarm bells all the time. And something similar has happened, it's a little bit of a detour here, but I think it's a similarity. We have this phenomenal stress response system in our brain. The immune system is a stress response system. We have another stress response system in our brain, which has saved our species over evolution many, many times. Not just ours, but every animal has that same system. It's the fight and flight response, and so today, we don't have these kind of stresses. At least for the majority of the population.
Still goes on in the world, obviously to a large degree. But in developed societies, it's much less common, but what we do have is a chronic exposure to an increase in level of stress. And that comes together with this more conservative stress response system in our brain, which triggers the alarm bells now constantly and similar what the immune system does. We have two systems that developed in evolution, that the modern world, become what we call maladaptive. They start causing diseases rather than protecting us against them. So I think that's what we're seeing. And they interact, this chronic stress interacts with the poor situation, the compromised situation in our gut level.
SHAWN STEVENSON: Yeah. You did highlight that as well in the book about stress, even acute stress, creating disruption with our microbes, but now we're just living in a constant fever, like a low-rate fever of stress. And I wanted to ask you about this, because I've been staying on top of the data since the very beginning. It's really about the questions you ask, and now we've got papers on the psychosomatic effects of COVID-19 for example, and I know for certain, and again, I could see this coming from a mile away, that there's a difference between healthy caution, being conscientious, and being inundated with fear. And there's been such a campaign of fear that none of us have seen before in our lifetimes, and to the point where people of course just feeling very paralyzed and disempowered, and I know for certain that that has had a major impact on our immune system function, but now you even bring to the forefront that this even disrupts our microbial function, which is really the house in which our immune system is existing in the first place.
DR. EMERAN MAYER: Yeah, and so this whole idea of how stress, acute stress, but putting it in a somewhat different way, but you call it disruptive, so acute stress leads to this up-regulation of the immune system response to defend you against... In this particular situation, chronic stress often goes in a different direction, and it's really important to realize stress is not just something that happens at your brain level, it's almost like if a mirror image of that state at your gut level, and every part of you got peristalsis or contractions, the secretions, fluid, acid secretion, mucous secretion, everything is affected by stress. If you take a stressed individual, either with an acute severe stress or a prolonged chronic stress, and you could characterize all the systems in your gut, they'll all be altered. And so not only the habitat in which the microbes live in is altered, but also some of these neurotransmitters, the stress mediators affect the microbes directly, they have receptors for our own stress mediators. So, it changes their behavior as well, it makes them more aggressive.
So, if you have an enteric infection and you're in a chronically stressed state, and so this is a very common thing, so people go to Mexico, get a GI infection. Different studies... If people go to Mexico when they're really stressed to distress, and they get one of these infections, it takes long, it lasts longer and it's more severe, as if somebody is in a completely relaxed state to go on a week to Chicago or somewhere.
SHAWN STEVENSON: Get that south of the border surprise?
DR. EMERAN MAYER: Yeah. And it's clearly a reflection of what happens in your brain, ongoing. We knew this for a long time, but now we know the microbes are affected equally in a direct way of changing their behavior, their gene expression, but also changing their habitat and their... So, we know we lose certain active basil during stress, and that has consequences downstream, but we also make individual pathogens more aggressive to attack our gut and interact with our immune system.
SHAWN STEVENSON: Yeah. So this should seem obvious again at this point, I think I've said this several times during this episode, but it's clearly, now we have some peer-reviewed evidence coming out that it's created worse health outcomes for us when we come into interaction with viral strains like COVID-19, for example, we should be stacking conditions in our favor to have a more favorable response, because we're going to be exposed to novel things, like this is just one, and yet the way that we've gone about this, I really think that we're kind of set up for worse health outcomes, like we as a society, we're even less healthy than we were at the beginning of this, more sedentary, more abnormal sleep patterns, eating more processed foods, we've gained more weight, the list goes on and on. And now I would really love to circle back because you said this term, and it burned me a little bit when you said it, because it really does fit, and you said warfare. And putting it in that term is, it can seem a little bit inflammatory, but it sort of is because we're going to war with the environment around us to destroy all of these microscopic organisms, not understanding that we're made of microscopic organisms. And in a sense, this is like war against ourselves, and we don't even realize it.
And I was watching this commercial the other day from... It was one of the big airline companies, and they were just smiling and showing how they're spraying the planes down with the electrostatic sprayers and all these chemicals, and they're like, "Look guys, look how safe it is now." And I can't help but wonder, what is that going to do to our microbiome? And it's not just rooted in our gut, as well, we have microbiome in our lungs, we have our skin, the list goes on and on. And we don't know what these things are doing to us, in this effort to defend us from something, kind of abstract and knowing that our bodies would be better defended if we had a healthier microbial cascade against anything we're faced with. I would love to talk about now, what are some of the things that we can do to address this? And going all the way back to, for us, for kids and coming up in a sterile environment, there's a time and place to use some hand sanitizer for example, but having it at the doorway and doing it 12 times a day, maybe it might be overkill, literally. Because we have to have a healthy interaction to develop and support our immune system. So, whether it's connection with people, whether it's being more judicious in our use of all these sanitation practices, what are some of the things that we can do to help to rebuild and fortify our immune system and our microbiota?
DR. EMERAN MAYER: Yeah. So certainly, in terms of the environmental exposure to microbes being in Spending more time in Green Spaces, and it's something that has happened automatically, it was a good thing that more families have selected or decided to have pets at home. So, pets are definitely one source of microbes that infants, or any animals relief, and it's unlikely there will be exposed more to farm animals, nobody's going to move. And even though some people may want to think about this, spend their vacation on a farm, when they have young kids, have their kids play in soil and natural... I think in cities that is mainly in park spaces. Diet-wise, clearly the biggest variety of plant-based foods, which more or less forces. They got microbiome to come up with all sorts of microbes that are specialized on these different fiber products, and polyphenol products from the plant, so the more diversities, the more you very force your microbial ecosystem to be diverse. I would say the use of disinfectants and... They will certainly go down from the extreme situation initially so; my wife came home from shopping and wiped every...
SHAWN STEVENSON: Yeah, my wife too.
DR. EMERAN MAYER: Food item, which is a terrible thing because food is a big source of beneficial microbes, not just in yogurt, or in fermented products. But if you look at the studies on an organically grown apple, there's a huge amount of microbes on that Apple when you... So many of our apples, obviously, they're polished and waxed and everything, they don't have this anymore, but to find the balance between being careful and people still talking about, we're not completely through this pandemic there may be variants. So, this is what you talked about earlier, this constant fear that's implanted in our brain, this may not be over, there may still be... So, we'll continue to be extremely hygienic. But I would say from diet mindset, as we talked about stress is definitely something that is almost as bad on the microbial, and gut health as diet is. And exposure to sources of outside micros from our... The food that we get, the people we interact with, physical touch definitely has not changed in families, but has changed with other groups, social groups.
We actually don't know what the impact of all the things we did during the pandemic had on our microbiome, I don't think we know the studies that looked at people that stayed healthy. Before the problem started to now. Did that lead to a decrease in our diversity? And will there be a delayed increase in all immune diseases? Will this boost a... But it's not easy, we more and more people live in big cities, in apartment, you take a place like New York City in small apartments. And it's not easy to sort of come up with, "Well, let's go back to the way it used to be that you played out in nature." And it was easy to access the healthiest food. It's not that easy, I think it takes a real conscious effort by people to do that. If you need the supplements, and this is something that a lot of people started a huge business during the pandemic, it's strength in our gut immunity. If any of these things really have a significant benefit on this problem, but honestly, I doubt it. It may in the future be, maybe things like polyphenols supplements that may have a benefit, we don't know that yet, but...
SHAWN STEVENSON: And that's even addressing it more at the root, which is the polyphenols feeding the microbes.
DR. EMERAN MAYER: Yeah, yeah.
SHAWN STEVENSON: But you go through, and you talk about this, there's been a major shift in awareness of the importance of probiotics, for example. And so, people just, "I just need a probiotic." But there's very little clinical evidence that they are effective, especially when people are maintaining and doing the same things they were already doing, like this magical pill is going to fix the problem.
DR. EMERAN MAYER: Yeah, this is a very important point. If you maintain your lifestyle the way it's before, and then you think you are now taking this probiotic that has 10 different organisms in it, in billions of concentration...
SHAWN STEVENSON: Yeah, 75 million, billion strains if you will.
DR. EMERAN MAYER: Yeah, if you think that that counteracts your lifestyle impact on gut immunity, and gut health, it's a pure placebo. That if you change your lifestyle, and you add certain supplements. I've still gone back and forth with this. To further enhance it, some of these anti-inflammatory substances like turmeric, or certain polyphenols.
SHAWN STEVENSON: And green tea, for example.
DR. EMERAN MAYER: Or green tea, there may be a benefit to it. But as you said, the scientific, we don't have the scientific studies. And we may never get them because these companies sell enough of these supplements without science. It's almost like something people willing to spend a lot of money on many of these things without ever having seen the evidence.
SHAWN STEVENSON: Let's talk about how something like intermittent fasting affects the microbiome.
DR. EMERAN MAYER: Yeah, so the interesting thing comes back to one of the things that I promote in the book, it's important what do you eat and where the food comes from, and when you eat it? It's really these three criteria. There's been a lot of studies in animals, in mice, on longevity and on metabolic health over three decades. All of which pointed in a beneficial effect of intermittent fasting. There's some human studies, growing number of human studies now that try to demonstrate that that works in humans as well, and during the study period, many of these are effective, decreasing inflammatory molecules in your body, weight loss. The problem with most intermittent fasting is that it's pretty not practical for the majority of people, that's what I would say. And the reason that if you follow somebody after a year, most people have regained their weight and have switched back to their old metabolic derangement. So, one of those techniques is time restricted eating. I find the most attractive and can't back it up with a ton of human research, but it's certainly practical, so we've done this in our own family during the pandemic, where you could experiment with this better because you didn't have to commute and everything. And so, we basically compressed the time where you put food into your intestine to eight hours or less and leave it empty for 16 hours.
That has a lot of theoretical benefits just on the gut itself, this having an empty gut will trigger, will completely switch the contractile activity of your gut, pair sources from a pattern where you grind and go back and forth and maximize absorption to one's pattern that goes, big contractile wave going through your gut from esophagus to the end of your intestine every 90 minutes like a clock work. That's where you want the most important mechanism to keep microbes, high density microbes out of your small intestine chances prevents what now is, received a lot of attention to SIBO, small intestinal bacterial overgrowth. So, it swipes everything down into the colon where most microbes belong to. So, it does that. At the same time, there's a wave of secretions that goes with these contractions, and so that alone is almost certainly beneficial for your health, for your gut microbial health, and your gut health and anti-inflammatory. So now we know from studies at Weizmann Institute that you mentioned that there are variation of how close the microbes get to cells that line the gut into the immune cells, or the distance between them and the mucus layer varies between day and night. And the longer the gut is empty, you have this more beneficial interactions of the microbes with the gut as opposed to when you feed it.
It's also something of our modern lifestyle that we have shortened that empty period by snacking, staying up till midnight or later, snacking during that time, and really reducing that window of when the gut is empty to just a few hours. So, I would say, and there are enough encouraging studies from mice. For example, one of the most impressive mouse studies is that they put mice on what's called a cafeteria diet, it's high fat, high sugar, where they gain a lot of weight and develop metabolic abnormalities. If you give that exact same diet with the time restriction, just in the eight-hour period, and honestly in a mouse it's kind of opposite because they are active during the nighttime, but it's the same time windows. If you give this in a time-restricted fashion as opposed to letting the mice have access to it all the time, the mice that eat the same amount of calories during this time-restricted pattern will not gain weight, will lose weight and will be metabolically healthy as opposed to the others. So that's very one of the strongest piece of evidence, and there's now evidence from some human studies, not 100% consistent, that that's the case in humans as well. And it makes a lot of sense. It's returning to our natural diurnal cycle really in terms of our food intake.
SHAWN STEVENSON: You just said something really remarkable, which is the same amount of calories consumed, but in that shortened window, it has this kind of protective effect in a sense. But I think it's beyond a protective effect, but there's these beneficial things that happen. You know this as well, but I don't think we've made the connection to how our gut and our microbiota are influencing the increase in BDNF, the increase in autophagy and all these things. It's really rooted in what's happening with our gut, like signing the check for these things. And you also mentioned staying up late. And I love that you have this in the book as well, because it's not just about our food, which you repeatedly throughout the book talk about real foods kind of functioning as this prebiotic source for our microbes to flourish. So real whole foods, a lot of plant-based foods, but I know you don't know this, but in my first book, Sleep Smarter, and this came out, I think it's about five years ago now. There's a chapter called Fix your Gut to Fix your Sleep, and I have many of the same tenets, which it's not trying to throw a pill at it, but what are some of the foundational things?
And that's what I want to ask you about this because, how in the world can our sleep patterns influence what's happening with our gut? Because one of the things that I was kicking around at the time was that it seems to be like there's a changing of the guard that kind of takes place with our sleep patterns, with what's happening with the activity in our microbes. Kind of like our microbes need sleep too or they need rest too, in a sense.
DR. EMERAN MAYER: Yeah. Certainly, we know that during REM sleep, with these different sleep phases, and during REM sleep there's this massive activation on the autonomic nervous system that affects all parts of our body. The heart beats faster and blood pressure goes up, and that also affects the GI tract. And so, this normal cycling between REM and non-REM sleep is definitely something that the microbes experience in a significant way, and which will affect... So, the people at the Weizmann Institute call this the geography of the microbiome. How close they get to the gut wall and how much they're able to affect gene expression in intestinal cells, and immune cells which then goes from the gut to the liver and affects metabolism in the liver. So yeah, it is kind of remarkable when you think about it, is that REM sleep and we've had these vivid dreams. The only reason we don't wake up is because the brain inhibits our muscular system at the same time, but it's as if we are in very emotionally arousing situations, several times during the night. So clearly what we know about microbial changes during emotional situations, that happens during the sleep just as it does when we're awake, we just don't know about it.
From a general standpoint, one property of healthy ecosystems are temporal oscillations or variations. So, the healthier a system is, the more regular are the oscillations, and so the renal variations are the most important ones for life on earth. But then there's the other frequencies of oscillations. Food intake, and I think the more that we stick to these natural rhythms, the better it is for the ecosystems inside of us as well. The thing that we do sitting in front of the TV at night, it's not by coincidence that you're being bombarded by all these food advertisements, snacks, unhealthy foods, it's not that...
SHAWN STEVENSON: Yeah, there's not a broccoli commercial on any night show.
DR. EMERAN MAYER: Yeah, no no. And you see these till midnight, and we know that that influences behavior, you go to the fridge when you see this, and you feel like you want to eat something. And ironically, at the same time, you see the commercials for how to treat your autoimmune diseases and your hyper-immune related diseases.
SHAWN STEVENSON: And your erectile dysfunctions.
DR. EMERAN MAYER: So, you get both of those things at the same time, it's ironic. You can actually learn a lot about how our society has moved away from encouraging a balanced lifestyle, just watching the commercials, what goes on there, because it's really smart people that are behind these commercials.
SHAWN STEVENSON: Right. And it's written, it's right there, right in front of our faces, but we don't really see it anymore. It's just we kind of see it as normal. So, picking up from that, we've got this powerful interaction between the health of our gut and influencing our sleep, and our sleep also influences the health of our gut. So, these are deeply interacted and have a deep interactive relationship. So, to put it like that. And one of the little fascinating nuggets, I'm just going to throw this out there. When I was in my university classes, I was taught that melatonin was produced in the pineal gland. That was it. Really that simple. But more recently, now we've seen that, and again, peer-reviewed evidence, there's upwards of 400 times more melatonin in our gut than in our brain at any given time. And you could even have your pineal gland removed, which I don't recommend by the way, but your levels of melatonin will still remain relatively consistent in your gut. So, the story is so much bigger. And I love that. I'm so grateful to have you on, because you are somebody who is truly a pioneer. It's 40 years you've been in this space and before we got started, I was like, "People probably thought you we're a little crazy talking about these things and this interaction."
And now to see your work and all the things that you've planted start to sprout out throughout so many different areas of health and how everything is interconnected. What I know is going to happen is we're going to see more work being done around heart health and the gut. Around lung health and the gut. Around brain health and the gut. And with your last book, you really focused on the gut-brain connection, and now in this book, the gut immune connection, and you didn't know the pandemic was going to happen, but you got to work on this subject matter because it is that important. So much of our immune system is rooted in our gut health, and the last thing I want to ask you about is, the One Health concept that you talk about in the book. Can you talk about that?
DR. EMERAN MAYER: Yeah, the One Health concept, it's the last chapter of the book, not by coincidence but going through all the individual systems. You ultimately, if you realize this is all part of a... Health and disease is all part of... It's best understood as part of a systems problem, that at multiple levels, this global system, this One Health system can be affected and then you have a ripple effect. So, if you start out with gut health, yeah, it's the health of the microbes and the way they interact with the immune system, but then you realize it's heavily influenced by what we feed our microbes, and then where does this food come from and what happened? The way this food was produced, we talked about this a few times, the microbes in the soil, they affect the nutrient content of the plants and how that benefits our microbes, to understand gut health and our brain health. So, we think they're all different things in medicine, there's specialists follow these separate entities, but really, I think you have to look at all the other aspects that are related to this.
The health of our environment that has affected the health of the soil, the health of our farm animals, and ultimately the health of the planet with climate change. Each of these things are in some ways interconnected, and I've cited one study where they looked at microbial, interactions of microbial systems in different parts on animals in the soil, on humans, different parts of the water. And you can create a network of all of these microbes that in some ways are interacting with each other. And given the fact that they have millions, or hundreds of millions of genes that can do all kinds of things. And so, it gives you this idea there's one underlying system that is being compromised now that creates disease states at multiple levels. And unfortunately, we live in a time where we see them all now, if you look at it with open eyes from our gut health to our brain health, to soil health, to plants, animals, and the environment. I think this is something that should be taught to children, early in school, this interconnectedness of all these elements, that they all play a role in our health, so if you're concerned about the environment, you do something for your own health as well. Same thing, if you want to create the optimal diet and environment for your microbes, you need to think about the environmental health at the same time.
So, this term has been used, has been created. I forgot now where it first came from, the One Health where it was animals and humans. But I think it goes much further, it really links every ecosystem on the planet together. And I spent a whole chapter in the book about explaining this whole network science that's beginning to explain this on a scientific level, and I think this is moving so rapidly in the scientific field that this will impact our understanding in medical textbooks, medical teaching in 10 years by the time it gets into the textbooks, into the curriculum. But it will definitely change the way we look at health in general.
SHAWN STEVENSON: Yeah. It takes time, and it's thanks to people like yourself putting the data together, making it to make sense and really pioneering against odds, against pressure and making it available. But like you mentioned, the change does take time, but it's happening right now. And so really grateful for you putting this together for everybody. Can you let everybody know where they can pick up your book and just anywhere, they can get additional information?
DR. EMERAN MAYER: Yeah. So, they can order it from any book seller, as of Tuesday, June 8th, you can even pre-order if you can't wait till Tuesday. Now, more information on this whole topic that we've been discussing is in my website, emeranmayer.com. And when you go to the website, it'll ask you to sign up for the newsletter, for the free newsletter, which will deal with topics from the mind to the gut and to the environment to this One Health concept. It comes out every two weeks. And then we're visible on all the social media, but all this information is on the website, so anybody who's interested in knowing more about this, order the book, or order both books. If you haven't read the first one and go to the website.
SHAWN STEVENSON: Yeah, thank you so much. This is an incredibly important conversation and topic. And I think clearly based on the evidence you've presented, that dialing in focusing more on healing our gut, supporting our microbiome can really help to fortify our immune system moving forward. So, I appreciate you so much for hanging out with us.
DR. EMERAN MAYER: Well, thanks, Shawn, it was really a pleasure talking to you.
SHAWN STEVENSON: Awesome, Dr. Mayer everybody. Thank you so much for tuning in to the show today. I hope you got a lot of value out of this. One of the most mind-blowing statements during this episode for me, is when he said, "The fact that today, our citizens have uneducated immune systems." Now, if you think about that in the context of what does our society built upon? What is of the utmost importance in our society? It's education, education is the way to achieving your goals, education is the way to innovation, to changing society. But what about the education of ourselves? What about the education of our immune system? The very thing that allows us to exist, to have life, to aspire towards those higher order levels of education. We need to educate our immune system. And right now, we live in an environment that is taking away educational opportunities in the form of sterilizing everything, anything and everything around us. When I mentioned during the episode about the electrostatic sprayers on the airplanes, and the commercials trying to get people come back and fly with us, you see, we're spraying all this stuff all over the seats, all everywhere, all over this plane. Just like we're spraying your food, look, it's so safe and protected.
And not understanding again, what is the impact that is having when we inhale those compounds? Which there is a 100% chance that you are inhaling those chemical compounds, 100%. What is that doing to our lung microbiome? Do we know how is this approved to be safe? And he mentioned during the episode that some of the early data that has allowed such rampant use of pesticides, and germicides and rodenticides. The tens of thousands of chemicals that have been approved for use by the EPA, is studying the impact that it has on, directly on human cells. But also keep it in context too, when we're talking to, "Oh, it doesn't hurt our human cells." Those are short-term instances, what happens in long-term with cancer development, for example? Cancer takes time. For us to actually be able to "Catch Cancer", to be able to see the manifestation of a tumor. Sometimes it could be years in the making before you realize like, "Wow, something happened in that cell replication process, and now we have a cancer tumor that is developed." But the roots of it, we don't see that in the short term, but what he mentioned was, okay, so we've got chemicals that are approved because it appears they don't hurt human cells directly, but they definitely hurt our microbial cells that are truly regulating what's happening with our human cells.
The very root, the essence of who we are, the soil really, if we're looking at our microbiome, it's really the soil that our health is being grown in and taking away these educational opportunities in the form of sterilizing, these hyper-sterilized environments that we're literally, you were born into those conditions. But with all of the different cleansers and chemical products and compounds, sure, yes, we want to make sure that we're not interacting with pathogenic organisms. But we evolved, we got to this place as humanity, having a resilient, healthy immune system that interacts with these things and our microbiome, our immune system literally it just pops its color, just gives a little color pop and keeps it moving, it brushes it off. It brushes it off, or it interacts with the microbe, learns and becomes better, and then that's passed on to the future generations. What's happening to us now, we know this for certain, we're passing on poorer microbial templates, that download that we get from our parents, from the microbes to what's happening with our genetic expression, all of these things are shifting in negative ways right now, and the results speak for themselves.
Every single... If we're just talking about the domain of chronic diseases in the last few decades, the numbers have skyrocketed, heart disease, Alzheimer's, lung disease, liver disease, kidney disease, diabetes, obesity, autoimmune conditions, the list goes on and on and on. We've become a culture where sickness is the norm, health is abnormal, and then we're talking about a new normal. Yeah, it's been like that. This is the new normal, but it's not okay. We don't want this to be normal, I want you to strive to be weird as fuck right now. I want you to be super weird right now, we don't want to be normal, we want to be weird, we want to be the weird healthy people, until that becomes the norm again, when being weird is socially acceptable, which is being the best version of ourselves, showing an expression of humanity and health that we're given by birthright to experience these things, but we're lacking in these educational opportunities because we don't have our hands in the soil, we're not able, we're not interacting with other people and getting in close contact, that's training for the immune system, that's downloads for the immune system, that's getting new apps that do cool stuff, and we're not getting those opportunities.
We're less and less, we're more and more isolated, we're more and more isolated from our environment, and we are part of the environment. That's one of the things that I love about his book, he's talking about the biological systems understanding that we have in science right now, which is wholeheartedly looking at... Because our system has gotten to a place where it's zooming in so much that it's looking at the tiny minutia, there's this thing that we found, this tiny, not even microscopic viruses causing disease or this tiny, tiny bacteria that's causing a disease or fungi, and not seeing the system as a whole, we need to do both. And the whole is, we are part of the same organism, we are a part of this system of planet Earth, and that's a part of the system of the Milky Way Galaxy, and it just expands from there. We are a part, we're kind of like tiny microbes on the earth's cellular body. And how are we functioning? Do we have the self-fulfilling prophecy of killing all the microbes or killing the dangerous stuff that's going to take us out? Or are we functioning in relationship to expanding our health and wellness and supporting all the other microbes here on the planet and being healthy and robust and having good information that we're sharing and moving forward to future generations?
We are part of the cellular body of the planet, and so the faster we can get back into accordance with this, this is that ancient... Our ancestors knew this piece already, and we've gotten further and further away from this, and we think that we're separate in some distinct way from nature, alright? So, lacking education, not getting those interaction points to develop our immune system, but also miseducation. Alright, this is going to be the new album, Laura Hill is going to make a comeback, miseducation of your microbiome, is going to be the new hitter, it's going to be some hot singles, all that. The miseducation of your microbiome, by being bombarded with all of the synthetic chemicals that humans are tinkering with now. Just in the last few decades, we've never had these things, these exposures in any of human evolution, and now it's not just a little bit, it's a lot, in the air we breathe, the water we drink, the food that we eat, it's everywhere, it's really inescapable.
Even if you're eating the organic kale that you've grown in your incredibly, biodynamic gard, all the good stuff, all the good stuff you could name. Because of the environment that we're in, you're still going to be picking up, DDT. That's been in the atmosphere, and in the environment for decades. We can't escape it, but when are we going to say, enough is enough? And stop, miseducating our immune system with this hyper-exposure to the pesticides, herbicides, rodenticides, the chlorinated water, the list goes on and on. Are there better ways to go about these things we've accepted as normal? And absolutely, you know there is. That's the thing about us, we are innovative, but we have to pay attention, and realize that this is a problem, for the change to take place. If not, this is going to be business as usual, until we as humanity, are just a footnote in the history of this planet. We can change it, we've got the opportunity right now. We've got to start to pay attention to the things that matter, and start to work on this miseducation, the exposure to these things.
The stress as well as we talked about in the episode, "How that miseducates our immune system. How this miseducates our microbes." The effect that stress has on microbes, we have this data now, but this would seem obvious. This would seem obvious. And so, moving away from the miseducation, right now proactively being pro-education for our microbiome, being pro-education for our immune system, in a way that's real, in a way that is sustainable, in a way that's in alignment with life. And not treating symptoms superficially, with new, this drug, this injection, this treatment, all of these external things bypassing, the very interface of our bodies and our environment. Which the hub of that, is our gut. It's how we most directly interact with the world environment, that the world around us, which is putting things from outside of our environment, the food that we eat into our bodies. It's such an intimate act that intimate experience, and we're literally getting this to decide what we're making our bodies out of, what are we making our microbiome out of, what are we making our immune system out of, we get to choose.
So, there's a lot of empowerment here as well, but I hope that you've got a lot of value out of this episode, and if you did, please make sure to share it out with your friends and your family. On social media, you can tag me on @shawnmodel on Instagram and Twitter, and At the Model Health Show on Facebook, and of course you can send this directly from the podcast app. You could text it right to folks and share a little bit of inspiration, empowerment, education, and let's keep this momentum going. I appreciate you so much for tuning in to the show today, we've got some epic shows coming your way very soon, so make sure to stay tuned. Take care, have an amazing day, and I'll talk with you soon. And for more after the show, make sure to head over to themodelhealthshow.com. That's where you can find all of the show notes, you can find transcriptions, videos for each episode, and if you got a comment, you can leave me a comment there as well. And please make sure to head over the iTunes and leave us a rating to let everybody know that the show is awesome, and I appreciate that so much. And take care, I promise to keep giving you more powerful, empowering great content to help you transform your life. Thanks for tuning in.
Maximize Your Energy
Get the Free Checklist: “5 Keys That Could Radically Improve Your Energy Levels and Quality of Life”
HEALTHY MEALS EVERYONE WILL LOVE
The Greatest Gift You Can Give Your Family is Health
When you gather your family around the table to share nutritious food, you’re not only spending quality time with them - you’re setting them up for success in all areas of their lives.
The Eat Smarter Family Cookbook is filled with 100 delicious recipes, plus the latest science to support the mental, physical and social health of your loved ones.











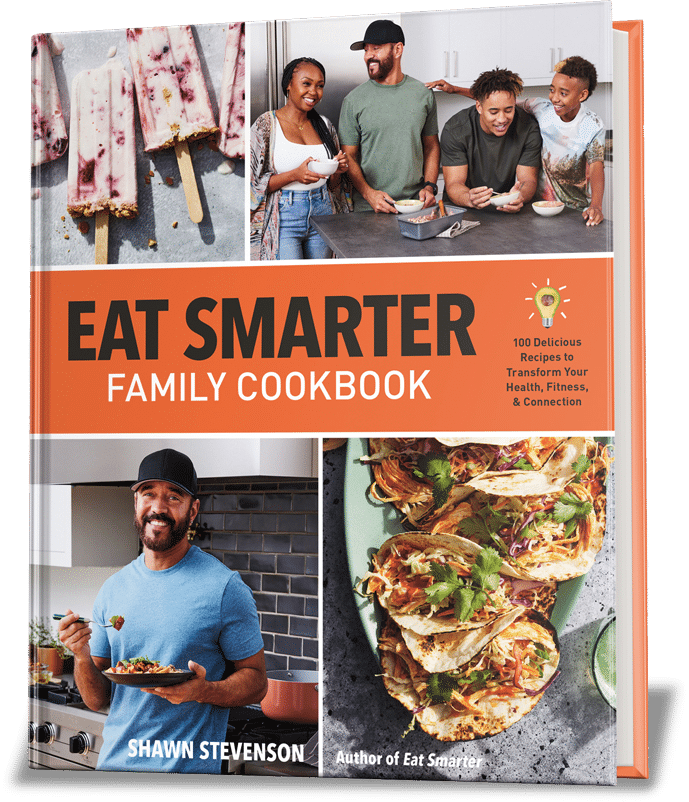
Share Your Voice
0 comments. Be the first to leave a comment.