Subscribe to The Model Health Show:
TMHS 531: Shocking Secrets About The Microbiome: Weight Loss, Dysbiosis, & More
One of the most fascinating and advancing areas of science is the field of microbiome research. Our understanding of our microbiome and its role has rapidly grown over the past few decades. The evolving knowledge of our microbial system shapes how we understand our biology, health outcomes, immune function, and so much more.
The health of our microbiome is linked to a myriad of aspects of our health, including our ability to fight viruses, our weight and metabolism, and susceptibility to major illnesses like cancer, autoimmune diseases, and Alzheimer’s disease. And while we do inherit some aspects of our microbiome, there is a lot that is within our control when it comes to determining our microbial health.
On this compilation episode, you’re going to hear insights and actionable tips from various experts on microbial health. This episode contains important information on how our microbes control different aspects of our lives, which medications can damage gut health, and which foods are essential for microbial diversity. You’ll learn why the microbiome is a main pillar of human health, and what you can do to positively impact the health of your microbiome. Enjoy!
In this episode you’ll discover:
- How our understanding of the microbiome has evolved over recent decades.
- The importance of having a healthy diversity of microbes.
- How our microbes can control our mood, appetite, and more.
- Why changing your gut bacteria can determine your fate.
- How long it takes the microbiome to recover from broad-spectrum antibiotics.
- What the most prescribed drug in the world is, and its negative effects.
- The role that stomach acid plays in regulating gut bacteria.
- Why it’s vital to be cautious about antibiotic use.
- How drinking enough water aids in proper digestion.
- The hidden cost of chemicals in modern agriculture.
- What it means to have a richness and diversity in the microbiome.
- Why gut health plays a critical role in preventing pandemics.
- What percentage of the immune system is located in the gut.
- The importance of recognizing bio-individuality when it comes to diet and gut health.
- What the five types of microbes are that comprise our gut ecosystem.
- The number one thing you can do to influence your microbiome health.
- Why allergies and autoimmune diseases are linked to gut damage.
- The connection between microbiome diversity and weight.
- How to improve the diversity of your gut microbiome.
- Specific foods you can incorporate to support your gut health.
- Why eating seasonally can impact your microbiome.
- The benefits of eating fermented food (& how many servings you should aim for!)
- Why sleep and microbiome are two of the main pillars of health.
- How soil depletion and nutrient depletion are intertwined.
- What postbiotics are.
- Why diets like low-FODMAP or SCD can damage mitochondrial health.
Items mentioned in this episode include:
- PiqueTea.com/model — Use code MODEL at checkout for 10% off!
- Beekeepersnaturals.com/model — Get a special 25% discount on natural remedies!
- Organifi.com/Model — Use the coupon code MODEL for 20% off!
- 5 Critical Keys to Unlocking More Energy with Dr. Steven Gundry – Episode 452
- Hidden Causes of Digestive Issues with Dr. Robynne Chutkan – Episode 251
- The Gut-Immune Connection with Dr. Emeran Mayer – Episode 487
- Our Misguided Battle Against Microbes with Dr. Will Bulsiewicz – Episode 440
- The Microbiome-Body Fat Connection – Episode 453
- Time Restricted Eating Transforms Your Brain with Dr. Andrew Huberman – Episode 524
- The Connection Between Microbiome & Lifespan with Dr. Steven Gundry – Episode 336
- The Plant Paradox by Dr. Steven Gundry
- The Longevity Paradox by Dr. Steven Gundry
- Dr. Gundry’s Diet Evolution by Dr. Steven Gundry
- Gutbliss by Dr. Robynne Chutkan
- The Microbiome Solution by Dr. Robynne Chutkan
- The Bloat Cure by Dr. Robynne Chutkan
- The Gut-Immune Connection by Dr. Emeran Mayer
- The Mind-Gut Connection by Dr. Emeran Mayer
- Missing Microbes by Dr. Martin J. Blaser
- Fiber Fueled by Dr. Will Bulsiewicz
- Eat Smarter
Thank you so much for checking out this episode of The Model Health Show. If you haven’t done so already, please take a minute and leave a quick rating and review of the show on Apple Podcast by clicking on the link below. It will help us to keep delivering life-changing information for you every week!
Transcript:
SHAWN STEVENSON: Welcome to the Model Health Show, this is fitness and nutrition expert, Shawn Stevenson, and I'm so grateful for you tuning in with me today. Many people regard this as the final frontier of health and medicine. Today we're going to be taking a deep dive into the universe of the microbiome and we're going to seek out counsel from some of the greatest minds and some of the most distinguished experts in the world in this field. So, this is something for us to really lock our attention in on, because as you're going to discover, our microbiome has a massive impact on everything from our immune function to our metabolism. So, this is going to be absolutely packed with insights about how this system, how this miraculous system of ours actually works, and some of the real practical things that we can do to fortify the health of our microbiome.
Now, before we get to our first expert, I've got to let you in on a little secret. One of the biggest things disrupting the health of our microbiome is something called dysbiosis. This is a condition where opportunistic or pathogenic bacteria begin to alter and shift the ratio to where they become more dominant in our gastrointestinal tract, causing a myriad of different health issues. So, gut dysbiosis can hourly cause gut-related symptoms, gas, bloating, pain, things of the like, but they can also have larger ramifications and often do, linked to autoimmune conditions, linked to issues with our cognitive function and so much more. So, this is a serious issue for us to really consider, and the biggest piece that we really need to focus on is removing the cause of the dysbiosis, and of course, adding in intervention, simple things that can help to fortify our gut health and support a healthy diversity of our micro-flora.
One of the things that I do specifically for that purpose is to make sure that I utilize something featured in a peer review journal, Nature Communications, and they uncovered that there's a unique compound called theabrownin, alright? Theabrownin, this might sound like your second-grade teacher's name, Thea Brown, Ms. Thea, Ms, Thea... Ms, Brown. Theabrownin, this is a compound uniquely found in this traditional ferment tea called Pu-erh, and it has some remarkable effects on our microbiome. The researchers found that theabrownin positively alters our gut microbiota and directly reduces excessive hepatic fat and also reduces lipogenesis, which means the creation of new fat. Another peer review study, this one was published in the Journal of Agriculture and Food Chemistry, found that Pu-erh may be able to reverse gut dysbiosis by dramatically reducing ratios of potentially harmful bacteria and increasing ratios of beneficial bacteria.
This tea is truly remarkable, but as with everything, the quality and the sourcing always matters, and today it matters more than ever. With its concentration of polyphenols, this tea is absolutely remarkable for gut health and for supporting our gut flora, healthy ratios of gut flora. But here's the key. The only tea that I use uses a patented cold extraction technology, extracting these bioactive compounds like polyphenols for up to eight hours using low to cold temperatures to really retain a lot of these compounds, so we get the maximum benefit. Now, this is a patented cold extraction technology, and here's the most important part, this company does something that most companies do not do, be it a tea company or otherwise. They do a triple toxin screening for one of the highest levels of purity, they're testing for pesticides, heavy metals and toxic molds that are common in teas, and most folks have no idea about this when they're seeking to get some of these benefits, but then they're getting nefarious compounds along with the healthy tea that they're trying to get.
I avoid all of that, and what I love most is that it's wild harvested, so it is absolutely teeming with these bio-active compounds, micronutrients, and what I'm talking about is the fermented Pu-erh from Pique Tea. Go to piquetea.com/model. That's P-I-Q-U-E-T-E-A.com/model, use the code MODEL at check out, and you get an exclusive 10% off for the Model Health Show audience. That's exclusive for us. It's the first time that they made a 10% discount available that you get for a lifetime every time you go to piquetea.com/model and use the code MODEL. Pu-erh is phenomenal. Their macha is just out of this world as well. Pop over there, check them out. Take advantage of this incredible Pu-erh for supporting a healthy microbiome, reducing gut dysbiosis. It's one of the things getting backed by real, peer-reviewed evidence, and you have access to this at piquetea.com/model. And on that note, let's get to our Apple Podcast review of the week.
ITUNES REVIEW: Another five-star review titled "Listen to this show, you'll love it!" by DooDoo DD. "Shawn, I'd never write reviews on anything, but your show is so good that I had to. I love it! So informative and so many life hacks that they're easy to put into your life right after listening. You talked on an episode about trying to be 1% better every day, using that compound interest to change your life and truly, your show helps me do that. Appreciate what you're doing."
SHAWN STEVENSON: Awesome, thank you so much for leaving me that review over on Apple podcast. That put a huge smile on my face, I appreciate it so much, and if you get to do so, please pop over to Apple Podcast and leave a review for the Model Health Show, and on that note, let's get to our topic of the day. Today we have a compilation of expert insights and advice on all things microbiome and who you're going to hear from up first is the incredible New York Times bestselling author, Dr. Steven Gundry.
Steven Gundry is a former cardiac surgeon and currently runs his world-renowned clinic in Loma Linda, investigating the impact on diet and health, and he is an absolute superstar, and Dr. Gundry actually pioneered infant heart transplant surgery back in the early '90s he was doing this work, and he's really made this major shift over to being an expert, one of the foremost experts in the world on the microbiome. And several of his New York Times best-selling books include The Plant Paradox, and also The Longevity Paradox. And here in this clip he's going to be sharing some insights with you about the recent discovery of our microbial genes, and also the surprising impact our microbes have on longevity, and some things that could be slowly destroying our microbiome. So, let's jump into this clip from the amazing Dr. Steven Gundry.
DR. STEVEN GUNDRY: Yeah, interestingly enough, 11 years ago, I wrote my first book called Dr. Gundry's Diet Evolution, and the subtitle was, "Turn off the genes that are killing you," and back in those days, we didn't know really anything about the microbiome, the bugs that live in us and on us, and I thought that it was actually our human genes that were controlling our fate. Fast-forward for this book, and the reason that book was called Dr. Gundry's Diet Evolution is because my thoughts have evolved, and quite frankly, if you're spouting the same thing, you said 10 years ago, I probably don't want to listen to you.
SHAWN STEVENSON: Right, it's probably broken.
DR. STEVEN GUNDRY: Yeah, it's guess what? Time marches on and research marches on. So, the fascinating thing is that our genes really have very little to do with what's going to happen to us. Huge NIH study recently published, that you're aware of, showed that of everything that's going to happen to us in longevity and diseases, our genes have only about 8% effect on what's going to happen to you and me. So that means 92% of the genes that are going to have an effect on you aren't yours or mine. They're actually our microbiome. So, we have trillions and trillions and trillions and trillions of bacteria, viruses, worms, protozoa in us and on us, and even though they have fewer genes per little bacteria than you and me, because there's so many of them, the microbiome actually has well over 260 times more genetic material than you and me.
And what's really cool, I learned this from a professor of microbiology in Paris a few years ago, and he thought, and I actually subscribed to his theory, that because what this huge resource of, if you will, computing power of genetic material that lives in our microbiome that reproduces constantly, he believed, and I back him up, that we uploaded most of our information processing. Just like we upload our information processing to the cloud, we uploaded or downloaded to our bacterial cloud because they've got more computing power, and it sounds kind of far out there, do-do-do-do... But I think he's right, because we now know that the bacteria within us actually control our fate. And it's really hard for a smart person to say, "Oh, come on now, these little one-cell organisms are going to control me?" But in fact, it's actually true because this is their home, and I like to tell people... You can get people to understand that we're basically a condominium for bugs, and this is their home.
And they're actually living in us at our request, and if we keep their home good, they'll keep us well, because quite frankly, if we're doing well, they'll have a great home the rest of their lives. And we'll probably get into this, but the amazing thing is you can take people who are 105 years old, very much like Edith Morrey, who are doing well, and look at their microbiome, which has been done, and compare that to the microbiome of 30-year-olds, and the 30-year-olds who are doing well will have the same microbiome as the 105-year-olds that are doing well. And it turns out most people when they... If they get to that age, have to have a youthful microbiome, or they're never going to get there.
SHAWN STEVENSON: So fascinating. And you talk about some of the studies that found that as folks are progressing nowadays, the average person, some of these species of bacteria, viruses, they're going extinct or becoming endangered in their microbiome. You don't see the same kind of cascade that you would see in somebody who's actually living a long time.
DR. STEVEN GUNDRY: Yeah, that's exactly right. So, it's this... Normally, we have this incredible rainforest of an ecology in our gut, and this rainforest... In a rainforest maybe there's 10,000 different species of plants and critters and bugs and every one of them is dependent on the other. So, we have an intense rainforest of bugs in our gut, and it turns out that that diversity, the same thing that makes a rainforest, has to exist in our gut and without that diversity, we're not going to make it very long. And what's happened, as you know, is that we pretty much throw napalm on our rainforest almost every day by the things we eat, the way our animals have been fed, the use of antibiotics, we could go on and on, glyphosate roundup. And so, it's no wonder that we may be living chronologically older, but in fact, as you started the show, our health span is actually decreasing dramatically.
The number of good years we have is going down and down and down. In fact, my generation, the baby boomers, are sicker on far more medications than our parents were at the same time period and that's actually scary 'cause baby boomers, we figured we were going to live forever and we're sicker than our supposed very sick parents.
SHAWN STEVENSON: Yeah. Man, this is so fascinating. And I want to talk more about some of the things that our microbiome does for us that we really don't think about, but first I just want to drive in this point because I remember reading about this almost two decades ago, the Human Genome Project, and we had this idea corn has 30,000 genes, these fruit flies have 20,000, for sure humans, we have 100,000 genes at least or something. We're so complex and dynamic. And then the research is done, and we have maybe 25,000 genes collectively.
DR. STEVEN GUNDRY: 20,000. Yeah. 20,000.
SHAWN STEVENSON: Right? Insane. First of all, we know that about two-thirds of those genes we can influence right off the bat with our lifestyle, these epigenetic influences, but my question is, what makes us so different? What makes us so diverse versus corn, which you would think doesn't have as much genetic information as we do?
DR. STEVEN GUNDRY: Yeah. Corn literally has far more genes than human beings. They have about 30,000 genes, and even the water flea, Daphnia, has more genes than humans. So, we actually are really fairly poorly equipped with genes, but what's fascinating is, again, we've traded our lack of genes in exchange for huge amounts of genes in our microbiome. And there's even one paper that I cite, which is fascinating. You can actually trace now from stool sample DNA of bacteria the immediate time, when humans split off from the lines of great apes that became chimps and gorillas and it was actually the change in the microbiome that actually determine that you and I are humans and not other great apes and you can actually now because the DNA is still intact in stools that have been fossilized, you can actually now detect that we're different because our microbiome changed and that is what made us unique.
SHAWN STEVENSON: Incredible.
DR. STEVEN GUNDRY: Yeah. It's like, "What?"
SHAWN STEVENSON: Yeah. It's so, so fascinating. It's so crazy one of the things you talk about and lovingly, affectionately calling these microbes our gut buddies and so I want to talk about some of the roles that they play for us because one of the things, for example, which I had no idea about for many years, they make vitamins and minerals in us for us and there's other kind of symbiotic things they do. So, let's talk some about that.
DR. STEVEN GUNDRY: Yeah, that's true. Without really your microbiome, a lot of the vitamins that we take for granted would never be absorbed or even manufactured in the first place. But what's really fascinating is we knew for many years that the gut was the source of a lot of important hormones that affect our brain, our mood, serotonin for instance, melatonin for instance, and we thought for years that this was produced by cells lining the gut, but we're now beginning to realize that these actual hormones are produced by our gut microbiome and you've got to have the right mixture of bugs to actually transform basic building blocks into, for instance, serotonin, which is the feel-good hormone.
So, if you've got bad bugs or gang members living there, they have no interest or ability to make these hormones. So, it's no wonder that if you've got a bunch of gang members in your gut rather than what I call gut buddies that you're angry, that you're moody, that you're anxious because that's actually a reflection of this really bad neighborhood that's living in you. And the other amazing thing is that they can actually control your food appetite. They can control what food you seek out and the gang members actually tell you to want simple sugars and saturated fats. That's what they live on. They actually can't live on complex carbohydrates, on resistant starches. The gut buddies love those, but the gang members, they can't live. So, the amazing thing is even obese people don't realize that I talk about in the book that the type of gut bacteria that you have determines whether you're going to be fat or thin no matter how many calories you actually eat.
There's now really cool research, that bacteria that live in the small intestine... Most people aren't aware that most of the gut microbiome research is done on colon bacteria, the stuff that lives in your large intestine. But years ago, I got focused on the small intestine, is kind of the forgotten area. Because most of the food nutrients that we absorb come out of the small intestine. And now some really ground-breaking research has shown that depending on the bacteria you have in your small intestine, bacteria are capable of extracting more calories from the food you eat and putting it into you, if they're bad bugs. If they don't exist, those calories don't go into you.
So, the old idea of calorie in calorie out is so flawed because it never took into account what the bacteria were doing with those calories. And as I talk about it in the Plant Paradox and again in the Longevity Paradox, you can actually do fecal transplants of fat bacteria into skinny mice. And there's one example of a skinny woman that I talk about in the Plant Paradox, who got a fecal transplant from a cousin who was overweight. And she was a skinny marathoner. And this woman gained 30 pounds without changing her diet. Because now all of a sudden, she had bacteria that were capable of extracting more calories and putting it into her without changing her lifestyle, just changing bacteria.
SHAWN STEVENSON: Again, blowing my mind out of my head. It's just so crazy. Of course, I went to a traditional university. And this was a thing that was drilled into us. If you want your patients to lose weight, have them to basically burn more than they're taking in. End of story. And it just simply is not like that. So many people have suffered and struggled doing that same thing and not understanding what's at the core of this conversation. There's so much I want to talk to you about. This is one study direct from your book. This was published in Nature, The journal, Nature. The make-up of an individual's gut bacteria was a better predictor of many health outcomes including blood glucose level and obesity. These things were better predictors than their genetics. And in other words, you have a better chance of sharing the same health conditions as your roommate or your spouse than your biological parents. And that's not because of luck or coincidence. It's because you have a similar gut bugs.
DR. STEVEN GUNDRY: Yeah, that's absolutely true. I was taught, of course, take a good family history. Because if your father had coronary artery disease or if your mother was a diabetic or if somebody had cancer, then there was a strong prediction that you would inherit that. No, it turns out when I take a family history, what I want to know is what were you taught to eat? What were you eating in the home? Because we now know that people who eat together actually share the same microbiome. And people who co-mingle share the same microbiome. And it's like the Nature study shows, it's your microbiome makeup that determines whether you're going to be obese. It determines whether you're going to be a diabetic. And quite frankly, probably determines whether you're going to get cancer.
SHAWN STEVENSON: Wow. Please hear this. This is so fascinating and so true. This is something that's been overlooked long enough.
DR. STEVEN GUNDRY: And what's so empowering about this information is you are not destined by your genes to have an outcome of your parents or your grandparents. You can change at any time into a totally different home for your microbiome. Though, you give them what they want, promote diversity of that microbiome by your food selection, and they'll totally change your fate. And that's what's so really cool. I changed my fate when I was 50 years old, approximately. And I was following my father's footsteps. Because genetically, I was developing everything that... What had happened to him? And now I have none of those things. I don't know if you know him, I'm almost 20 years older than that now. And you go, "I just changed my microbiome." And they went, "Hey, this is pretty good place to live. And we're going to kick out the squatters and the gang members, and spruce up the place. You got good bones here." Yeah.
SHAWN STEVENSON: Spruce it up.
DR. STEVEN GUNDRY: Yeah, spruce it up.
SHAWN STEVENSON: I love this. So, I want to talk about, obviously, some of the action steps that we can take. And there's so much in the book, guys. But before we get to some action steps, it's really... And this is just my professional opinion as well, is removing a lot of the cause. Instead of trying to do more stuff, let's just remove the things causing the problem in the first place.
DR. STEVEN GUNDRY: Correct.
SHAWN STEVENSON: And so, I'd love to talk about some of the things that are damaging our gut buddies, that are just rolling through doing drive-bys, just this crazy stuff. I want to talk about antibiotics really quickly. And then I want to talk about... I definitely want to talk about GMOs. Because it's one of those things where it's not a big deal. But you articulated it in such a way that it's just like, "That's why it matters." So, let's talk about antibiotics, then GMOs.
DR. STEVEN GUNDRY: Okay, so antibiotics. Broad-spectrum antibiotics came out actually in the mid-70s, mid-late 70s, when I was in medical school. And these were miraculous. Because before, we had to figure out what bacteria was causing an infection and then select an antibiotic that would work against that bacteria. And it was very time-consuming. And sometimes you never did figure it out. Well, when broad-spectrum antibiotics came out, it was a miracle because we didn't have to know what the bacteria was. We just gave you basically napalm. And it killed everything. Now, we were naive to think that it didn't kill everything in our gut. And so for the last almost 40 years now, we give broad-spectrum antibiotics just for anything, mostly for viruses, so somebody comes in with a cold or a cough, or bronchitis, most of these are caused by viruses that antibiotics have no effect on, but doctors, because patients are persistent say, "Oh, you know, here's a Cipro, here's Levaquin, your cold will be gone in a week and... "
SHAWN STEVENSON: Yeah, placebo effect.
DR. STEVEN GUNDRY: And there's a very good placebo effect. So this stuff is given away like candy, and that is like blowing napalm on our tropical rainforest, and some of the really scary data that's coming out of UCSF and Stanford, our gut microbiome may not recover for over two years after an initial course of antibiotics, and some people they've actually found only a single species in your gut two years after a course of antibiotics when there should be tens of thousands of species. So, it's just like the fires here in Southern California, people go, well, we'll just plant some new seedlings, and we'll have a forest again. No, it's going to take years and years and years to get that intense ecology of a forest. So just swallowing probiotics is just not going to do the difference.
So please, antibiotics are lifesaving, but we got to save them. But the other thing is, almost all of our animals that we eat, whether they're chickens, beef, pork, lamb, some fish, farm-raised fish are given antibiotics and they were given antibiotics primarily to make them grow faster. And this was discovered years ago by a veterinarian in the Midwest who was giving animals tetracycline, and he said, "Oh my gosh, you know, these animals make... Grow faster and bigger on the same amount of food if I give them a little bit of tetracycline. Wow, this is great news." Well, so the FDA approved antibiotics in animal feed for years and years and years, and only recently have stopped allowing that. So, it makes us grow faster but weak at a little dose of antibiotics every time we have a factory-farmed meat, because a veterinarian is still allowed by the federal government, if it thinks one bird is sick, it can dose the entire flock of 100,000 birds in a warehouse with antibiotics, and guess who pays the veterinarian? The big factory farms. So that's why this stuff still ends up in our food supply.
SHAWN STEVENSON: Up next in our microbiome master class compilation, we’ve got one of my favorite experts and people, Dr. Robynne Chutkan. Dr. Chutkan is a world-renowned gastroenterologist and author of the best-selling books, Gutbliss, The Microbiome Solution, and the Bloat Cure. She received her bachelor's from Yale University, and her medical degree from Columbia College of Physicians and Surgeons, and she completed her fellowship in Gastroenterology at Mount Sinai Hospital in New York. Dr. Chutkan has been on the faculty of Georgetown University Hospital since 1997, and she's also a former board member of the American Society for Gastrointestinal Endoscopy. Dr. Chutkan had been featured on the Today's Show, CBS This Morning, The Doctors, the Dr. Oz Show and so many other major media outlets. And in this clip, she's going to be talking about how common gut targeting drugs are actually exacerbating gut problems and damaging our microbiome, and how reducing sugar and improving hydration can radically improve your microbiome and overall digestive wellness. Let's jump into this clip from the amazing Dr. Robynne Chutkan.
DR. ROBYNNE CHUTKAN: And I'll tell you Shawn, I distinctly remember the first time I realized that these drugs that we tend to prescribe like candy were really a problem. It was about 15 years ago at a Food Is Medicine Conference, my friend Gerard Mullin, who's an integrative gastroenterologist at Hopkins, a great guy, he's got some great books out, he started talking about the effect of acid blockers on the gut and the microbiome. And think about it, a dozen years ago, 15 years ago, nobody really knew much about the microbiome, or rather we knew about it, but we didn't know how important it was. And I remember listening to Gerard's lecture and just being riveted and realizing we are actually creating disease with a lot of these drugs. So let me walk you through what happens when you're on an acid blocker, a potent acid blocker like what we call proton pump inhibitors, a little purple pill and others, and keep in mind that these drugs are amongst the most commonly prescribed drugs in the world.
Because when people have acid reflux and they take these drugs, these drugs really very effectively and efficiently block stomach acid, and what that means is you don't get that natural feedback that's so important from your body to tell you that something's wrong. When you're having a Porterhouse steak and mashed potatoes with cheese and a couple of scotches at 10 o'clock at night and you don't feel well, that's a really important sign, that's important feedback that your body is giving you to protect you from doing it over and over again. And so, when you remove that negative feedback, you can really induce some damage, so these drugs block stomach acid virtually 100%. And stomach acid is important for some really big reasons, number one, they provide the ideal pH to digest food. So, when you don't have any stomach acid you get maldigestion where you're really not absorbing and assimilating the nutrients properly.
And we know that because we know people who are on these drugs for years and years, or even sometimes for months can end up with iron deficiency, they can end up malabsorbing fat-soluble vitamins like A, D, E and K. And this can actually lead to osteoporosis and osteopenia and so on. So, this can lead to bone issues because you're not absorbing vitamin D and calcium and other things properly. So maldigestion is a big one. The other thing is that having an acidic pH provides an ideal pH for the digestive enzymes to work properly. So now the enzymes are trying to function in a different pH. And that's not quite ideal. But for my purposes, one of the biggest issues with them is that they cause an overgrowth of gut bacteria, because they transform the stomach from a pretty hostile acidic environment where excess bacteria don't like to hang out to a very friendly alkali inviting environment.
Now you have overgrowth of gut bacteria in the wrong part of the GI tract. Gut bacteria, really, as we go from north to south, from the mouth all the way down, the amount of gut bacteria increases. So, they should really be concentrated in the colon. But instead, you have increasing levels of gut bacteria in the stomach and the small intestine, and a form of dysbiosis called SIBO, Small Intestinal Bacterial Overgrowth. It's really an imbalance issue. So, these drugs can really create this problem, or they can compound the problem in somebody who has other risk factors like taking antibiotics, being a picky eater and so on. And I'm so glad, Shawn, when you talked about your story, you mentioned this sort of background of dysbiosis. Because I see that so commonly. People might be struggling with thyroid issues or lactose intolerance or celiac disease or chron’s, but there is a background of alterations in the gut bacteria and microbial sort of disarray, dysbiosis essentially. And so even if they remove the lactose or get rid of the gluten, sometimes they're still not better because they haven't dealt with the imbalance. So, it's such an important point.
SHAWN STEVENSON: Exactly. And of course, you address that so much in The Microbiome Solution. And you'd of course talked about it in The Bloat Cure as well, because it's not just, "We're going to go in here... " And I want to talk about this next, antibiotics and how this can lead to bloating. But just going in and kind of destroying the terrain, and that's going to solve your problems with something like SIBO or some other kind of infection. But we have to really focus on rebuilding with all the different stuff that we're exposed to kind of crowd out the bad guys in a way. So, let's talk about that next. Let's talk about how antibiotics can play into this whole equation.
DR. ROBYNNE CHUTKAN: Well, I'm so glad you mentioned the word terrain. It's one of my favorite words these days. And we're really referring to the internal ecosystem in our bodies, and primarily in our gut. And that soil needs tending the same way the soil outside needs tending. You would just go outside in your garden and drop some seeds in the ground and hope that somehow something useful grows. So, you really have to prepare the soil and cultivate it and think about the sun and the wind and the rain and what you're planting and when the best time to plant it is. There's really a lot of thought and preparation that goes into it. And the same thing, if your idea of remediating the problems that are going on or just to take a probiotic and call it a day, you're really not going to see meaningful re-population and regrowth. Antibiotics are really high up on the list along with acid blockers.
Because a typical five-day course of a broad-spectrum antibiotic, the type that you would take for a sinus infection, or a urinary tract infection can remove up to a third of your gut bacteria. And those species are really never coming back with the same vibrancy and intensity that they were there before. So, I like to use the analogy that it's sort of like taking a bath that's full of water, draining out all the water and then pouring a cup of water in which is your probiotic. And not to say that probiotics can't be helpful, but there's no probiotic out there that can completely mitigate the damage of an antibiotic. And so, the most important thing for people to know is that they have to use antibiotics judiciously. You can't just go eat some yogurt or take a probiotic and think that you'll be fine. So, you have to be absolutely sure that the condition you're taking the antibiotic for is absolutely necessary. It's not something that's going to get better on its own, or you can sort of watch and wait. You've got to be really, really, really sure that you need to take it.
SHAWN STEVENSON: Exactly, thank you so much for saying that. And again, if your physician is against this approach, you can always find another physician. Because the goal here is to be empowered. And your physician should be more of a coach to help you with these processes. And there's also testing that you can do to find out which antibiotic is specific for the thing that we're trying to target.
DR. ROBYNNE CHUTKAN: Absolutely. And so much of what people are being treated for are either self-limited things that will get better on their own or they're viral. And antibiotics, of course, don't work against viral illnesses. But we're in this sort of quick era of medicine where, "Here's a prescription. See you later. It's a seven-minute appointment." And so, the point you made is so important. We really have to be the advocates to be more empowered about our own health. And if you're having a monologue with your doctor where they're speaking at you rather than speaking with you, and it's not a dialogue, you probably need a new doctor. Gastroenterology is not complicated. It's plumbing. That's really all it is. And I laugh. I'm like, "Yeah, the really smart people in medical school go into nephrology."
So, we are plumbers, basically. And the goal is to get the products of digestion from north to south. From the mouth to the anus, out into the bowl. That's the goal. And when you think about it very simplistically, when stuff is dry and not in a liquid phase, it moves much slower. So that is again, one of those incredibly simple things of just people to drink more water. If you had a clogged pipe, you would run water through it. That's what you run through it, a thin liquid to try and clear it. It's the exact same thing in your gastrointestinal pipe. So, you need things to be in a liquid phase so that they can move efficiently from north to south. And most people don't drink enough water. And they take medications and drink things that dehydrate them, like soda and coffee and other kind of sweet sports drinks that work as a diuretic. And they actually pull fluid out of the GI tract.
And have a diuretic effect. So, it's so important to be drinking enough water, to be measuring how much water you're drinking. I tell people look in the toilet bowl. Look at the color of your pee. It should be... You should barely be able to see any yellow color. You really should have clear pee as one of the indicators. There are lots of other indicators too. We can look at skin turgor and different things and how people are sweating. But that's a really simple thing to do, is just you should be peeing frequently. And the pee should be clear. And you'll notice a big difference too with the ease of evacuation, less straining and so on with drinking more water.
SHAWN STEVENSON: Oh, my goodness. You just again, brought it back to simplicity. But I've got to tell you, and we've talked about this numerous times in the show, but folks would be getting upset because they start drinking more water and it's like, "I'm going to pee so much. Is that bad? Is that a bad thing?"
DR. ROBYNNE CHUTKAN: It's good. No, it's good. That's the point. It's inconvenient, especially when you got to unhook and unzip and unbutton. But it's so appropriate. And it's so necessary. And people spend all this time thinking about cleansing and detoxing.
SHAWN STEVENSON: Right, yeah.
DR. ROBYNNE CHUTKAN: That is one of the simplest things you can do to cleanse, and detox is to drink more water. You don't have to do some $1,000 green juice fast. You can, but just drinking more water really, that's what it's doing, it's really cleaning you out.
SHAWN STEVENSON: Yes, perfect. I love this. We've already covered so much ground, guys. This is just amazing, amazing stuff. But we've got so much more here as well. She's just a virtual fountain of information. Let's talk about... So earlier you mentioned some of the products that we might consume, and you mentioned it's things like coffee. But what about sugar? What about sugar? How can that lead to bloating?
DR. ROBYNNE CHUTKAN: Sugar is a really big one, because we talked about antibiotics and acids suppressing drugs as two of the main drugs that can disrupt the microbiome. Sugar is one of the main foods that can disrupt it because it leads to overgrowth of the less desirable species. Now, we tend to look at good bacteria in very black and white terms, as either good or bad. And it turns out that there's this whole concept of a pathobiont. So, a symbiont is a bacteria that is not going to do us any harm, and maybe it could do us some good. And a pathogen is a bad actor, so Ebola. Nothing good about Ebola in the body. But if you think about something like yeast, yeast get a really bad wrap. But the truth is, yeast are essential as part of the digestive process. The problem is when you have overgrowth of yeast.
So, you take an antibiotic. It kills off a lot of your healthy bacteria. There's a lot of room in the microbiome. And so, some of these species, like yeast proliferate. But the yeast themselves are not pathogens. They are pathobionts. Meaning that in the appropriate ratio and proportion, they're either benign are actually helpful doing a job. But when they over-grow, now it's a problem. And so, we see a lot of these organisms that are pathobionts, that get over-represented because they get preferentially fed by a sugary or starchy diet. And that's... So, a little bit of sugar is fine. And I always recommend that people use real sugar as opposed to artificial sweeteners. But again, it depends on your terrain.
So, if you are somebody who's plagued with yeast infections and bloated, and a yeast infection is a great sign that the terrain is off, then a more drastic elimination of sugar, or maybe a sugar detox, could be a great idea. If you're somebody who already eats a healthy diet, eats a lot of plant fiber and so on, and you're not... Your train is okay, you're looking to enhance it, you can probably tolerate a little bit more sugar. So again, it really depends on this idea that nobody should ever eat any sugar. I don't think that's necessary. But you do have to look at what's going on and really think about what you need to do to remediate it.
SHAWN STEVENSON: I hope that you are enjoying this microbiome compilation and as Dr. Chutkan just shared, sugar especially conventional, highly refined sugar, can set off an absolute rave by pathogenic bacteria in your gut. Alright, dun dun dun dun. It is going nuts in there. It's feeding the problem. And she's also one of those people... She's not saying, "Hey, we need to eliminate everything sweet. We need to pull it out." Oh, she's somebody who I know has been an advocate of like, "Let's upgrade. If we're going to use some sweeteners let's upgrade or bringing in and actually finding a way to fortify and feed our healthy, protective, probiotic, friendly flora." Now, myself, personally, I'm definitely not a fan of processed sweeteners, even if they're 'natural.' There is one sweetener that is noted to have a stabilizing effect on blood sugar versus other sweeteners.
And a study published in the journal, Food Quality and Safety, detailed how natural raw honey functions as a remarkable prebiotic that helps positively alter bacteria in our gut, our overall bacteria cascade and improve overall metabolic function. So, improving our metabolism by improving our gut health. Specifically, it's the oligosaccharides in raw honey that add this benefit, not to mention the incredible anti-inflammatory properties that the right honey has, being able to actually... Inflammation is one of the things that really terrorizes our healthy gut micro-flora. The word inflammation is derived from a root word, meaning to set on fire. And so, we might hear terms like inflammation and think, "Hey, it's no big deal." But this is one of the things that greatly exacerbates damage to our tissues and also accelerates aging. None of that is good. A study published in evidence-based Complementary and Alternative Medicine found that honey polyphenols able to reduce inflammation, including neuroinflammation.
It's that remarkable, it can even reduce inflammation in the brain, and honey polyphenols are useful, improving memory deficits as well, according to this study, and can actually act at a molecular level to help to heal our tissues. Now, what do I mean by the right honey? I'm not talking about the pasteurized heat-treated honey that destroys these metabolically active compounds. Honey is probably the most enzymatically active food substance ever discovered. And guess what's getting destroyed when it's heated. That's right, those enzymes, these enzymes are really these... At its core, these are proteins, but enzymes really act as catalysts that really activate and drive every single activity in our bodies, enzymes have to be there like these little keys that unlock processes.
And so, honey being this enzymatically active compound, this is why it has so many remarkable benefits. Now, when honey is heat-treated, you're losing a lot of this capacity, so that's number one. Number two, conventional honey is going to be picking up a lot of pesticide residues because of the environment that it's getting grown in, not to mention that you've got some other environmental pervasive offenders like DDT, "bad" bacteria like E. Coli, for example, when we're talking about helping to heal and restructure our gut to reduce dysbiosis and pathogenic bacteria, you can be picking some up if you're getting the wrong kind of honey. Also, heavy metals again, mercury, lead, arsenic, these are common things found in conventional honey. Getting your honey from a company that goes above and beyond to do third-party testing outside of their own domain for these nefarious compounds, and who are dedicated to sustainable beekeeping, we've got to commit ourselves to that because as you probably know, bees hold a powerful and important key in our food system, in our food supply, we've got to take care of these bees.
I didn't know I was going to rhyme, we've got to take care of these bees, it's truly of the utmost importance. So, helping to support sustainable beekeeping is one of the most important things for us to think about moving forward, this is why I get my bee products, including my Super Food Honey from Beekeepers Naturals, go to beekeepersnaturals.com/model. That's B-E-E-K-E-E-P-E-R-S naturals dot com forward slash model. Again, that's beekeepersnaturals.com/model, and listen, exclusive, they just bumped this up, they had a 15% discount, right now, it's 25% off right now. Go get yourself some of their Super Food Honey, their B. Smart Neotropics based on royal jelly, their anti-viral propolis spray, so many incredible things, and they're the best, period, end of story, they are incredible, go to beekeepersnaturals.com/model for 25% off. Now we're going to get to our next expert in this Microbiome Master Class compilation.
And up next, we have Dr. Emeran Mayer and he's the executive director of the G. Oppenheimer Center for Neurobiology of Stress and Resilience, and the co-director of the Digestive Disease Research Center at UCLA. He's also the author of the best-selling books, The Mind-Gut Connection and The Gut-Immune Connection. And in this clip, he's going to be sharing how our treatment of the soil that we use to grow our food is dramatically changing how our microbes are being fed, or should I say not fed. He's also going to share what richness and diversity means when it comes to the microbiome, and how our microbes influence our immune system in the context of COVID-19. So, let's jump into this clip from the incredible Dr. Emeran Mayer.
DR. EMERAN MAYER: Yeah, this is a big thing. So industrial agriculture essentially is chemical agriculture, it's gone from an organic agriculture that is indigenous people use that way with natural fertilizers from the farm animals that go back into the ground. So what modern agriculture has done, particularly or increased in the last 75 years since World War II, to increase productivity and output and feeding the world, and that actually has been successful, but at a very high cost, because putting all these chemicals, not just into the soil, has killed a lot of the microbes, similar what we have done with antibiotics in humans has a good side, wonderful side, but at the same time, has a hidden cost that we now realize.
The second thing is by killing a lot of the microbial ecosystems in the soil, the plants have lost the ability to produce their own medicine, which is a group of molecules called polyphenols, and that's a whole topic for... We could talk about this for an hour, one of my favorite topics, that the soil microbes stimulate the plant roots to produce these molecules, to then transport it up the stem of the plant into their leaves into their fruit and defend them against any kind of stress. So, it could be chemical stress, it could be insecticides, it could be drought, anything that stresses the plant generates a signal down into the root system to communicate with the microbes in the soil, which then stimulates this medicine production, this phytochemical and in industrial agriculture, that's greatly diminished. So that results in the need for pesticides and insecticides, because these plants are no longer... They grow like crazy, as long as you kill everything else around it.
SHAWN STEVENSON: Right. They're not adaptable.
DR. EMERAN MAYER: They're not adaptable. And so, you start off with killing the microbes in the soil, then you have to start killing all the bugs and the pests that could compromise this plant because it's no longer producing its own medicine. And so that created this vicious cycle that we're now producing plants that look beautiful, and you go to Gelson's or Whole Food Market and see these beautiful looking... But the nutrient content is not the same, 'cause these molecules that protect the plant at the same time are the main components of the nutrients that are contained in the plants, and when we eat these plants a big health benefit is not just the fiber, but it's also these plant medicine molecules which...
SHAWN STEVENSON: Like polyphenols.
DR. EMERAN MAYER: Like polyphenols. And so, we're now eating a diet that's really greatly diminished in this. And so industrial agriculture, I like to call it chemical agriculture, has really played a major role. And then we're kind of coming back to realize that, now there's some pioneers that promote this regenerative, organic agriculture. Regenerative means you put things back into the soil, you don't just constantly extract things from it, but you put it back so the microbes can grow, and you restore that ecosystem. So, there's people like the people behind the Kiss the Ground movie. It's a good example. Yvon Chouinard from Patagonia is another example who's really been pushing this concept. Sir Ryland Engelhart is the mind behind the Kiss the Ground group and the movie.
So, there's a growing number of people, and they have a plan to really change agriculture back into a regenerative organic system, which would solve a lot of problems because one of the things also... So, we didn't really know what some of these pesticides and insecticides do to the plant and then to our own, because we eat the plants, to our own microbial ecosystem. Just for glyphosate to get FDA approval, they only had to do a few studies, short-term studies, in cultures of cells, and they found, in human cells, and they found that glyphosate exposure... So, the substance that is roundup, that glyphosate exposure did not really affect human cells because human cells don't have that shikimate pathway to metabolize it. So, they concluded from a few short-term studies, it's safe, it doesn't affect human cells.
SHAWN STEVENSON: Oh, this is fine.
DR. EMERAN MAYER: This is way before the microbiome science came around.
SHAWN STEVENSON: Right. Right.
DR. EMERAN MAYER: So, in the meantime, we know microbes can break down most chemicals of interest, including glyphosate. And believe it or not, there's very little science on that. And I don't know, it almost seems like... I hate to be a conspiracy theorist, but it's almost like if that science is not supported, it's not like... You won't get funded to doing this. 'Cause the commercial interest and the lobby behind that industry is so gigantic that... I don't know, I don't want to get into the political implications of this, but there's certainly... It's very surprising that at a time where we're so conscious of the health, the gut health and everything, that there's not a flurry of studies that show definitely the glyphosate does harm, not just the microbiome but also, secondarily, our own health.
SHAWN STEVENSON: Yeah. The regulatory systems are really backwards because we're trying to prove that they're hurting us instead of proving that they're not hurting us, it's really backwards. And it should be obvious, again, these are newly invented compounds. With the EPA, for example, there's like close to 40,000 chemicals approved for use in fertilizers, it's so many. It's insane. And once we get in this conversation... So, I mentioned earlier about directly damaging microbial gene expression, but that's just one part of it, because... So, the ingestion of these chemicals can disrupt our microbiome, but also the lack of key nutrients. Even if we're eating organic, the foods that we're eating today are lacking on these nutrients that feed our microbes. And so, this is what I want to ask you about next because we've seen a direct impact, and you highlight this in the book, and it's so important. The direct impact is a vastly declining richness and diversity of our microbes. So, can you talk about those two different things, and the current state of our microbes versus people who are eating more of a normal diet?
DR. EMERAN MAYER: Yeah. So just to explain these two terms, and they are important, so that applies to any ecosystem. So, the richness and diversity applies... It's not just for the microbiome, but... So, diversity means how many different species of organisms are there? So, a high diversity would be something... If you extrapolate this to a city, if you have one couple from Latin America and one couple from African-American and one couple from Asia and the rest is all Caucasian, so that's a diverse ecosystem because you have four different... And it could be a more diverse... But it's not necessarily a healthy ecosystem because that one representation of one species is not sufficient, you need a richness, you need... If you divide up the population, you would want to have 25% of each of these populations populating that ecosystem, and that's the richness. So, you need the richness and the diversity in order to get...
So, the main property then of such an ecosystem is... It's resilient against perturbations. It's very... Anything you do to it, it will bounce back, it will not... Something that will break down. And it will be resistant to change, and that's clearly a property of our own microbiome. It's a good and a bad thing. The good thing is if you eat something or get a giant infection or eat something bad or have a stomach flu, it doesn't knock out your system, it always comes back. And it's the same with if you take an antibiotic once it doesn't knock out your system, even though you kill or suppress all the organisms, it comes back because of its resistance or resilience to perturbation. The bad thing is, if you want to restore a sick microbiome, like we do in... So, there's a lot of attempts now with this fecal microbial transplant, because we can do this in mice, artificial models that you take a rich, diverse, healthy microbiome and put this into a mouse gut, you can do all kinds of things. You can make an obese mouse lean, you can make a depressed mouse normal behavior, but you can only do this because these mice start out, these laboratory mice, without having any microbes. The so-called germ-free mice.
So, in a situation like that, yes, you can change it if you put some in, but even in people that have a compromise microbiome, it's still resilient. So, it won't allow you to do that, it will not... There's very few conditions, there's actually literally just one condition, where a fecal microbial transplant in humans has really worked. And that's because, again, the resilience and the resistance for change. Our microbial, this ecosystem has been declining in both diversity and richness, so we are losing... And that's just kind of perpetuated through generations, it gets worse, a little bit worse in each generation. We've been losing a lot of this diversity and richness, and some strains have disappeared that you find in populations like hunter/gatherer remnants in the world. So, we've lost a lot of these species, not species as much, but strains, and this is continuing. If you don't change something dramatically in how we interact with the environment and with our food and with the chemicals we use, that this will continue, and some people have predicted it will lead to massive pandemics because it makes us more and more vulnerable to infections and... It's interesting, so a book came out a few years before the pandemic, Missing Microbes by Martin Blaser, and in his last chapter, he talks about this, the threat of pandemics. This was way before the actual pandemic we're in now. And so, we got a taste of it. What can come, even worse in the future, I think.
SHAWN STEVENSON: This is really getting to a place of something very visceral for us because we're seeing again, firsthand, which you can really see coming from a mile away and understanding that truly a big regulatory force of what we see as our immune system has so much to do with the health of our gut. And in the book, you also detail, again, there's a decline... If you want to look at it like an analogy of a rainforest and this loss of species, and how does that affect other species and the richness and diversity, and we've been losing these strains. Many have gone extinct; many are on the endangered list. And so, we still have an opportunity to kind of turn these things around, but I sent this paper over to you and I knew that you had already seen it, but I wanted to ask you about this because you also mentioned with the richness, it really holds within it its ability to bounce back. When we have any kind of intrusions or anything, any abnormalities, it's the ability to bounce back.
And this recent paper was published in the journal Gut and is titled, Gut Microbiota Composition Reflects Disease Severity and Dysfunctional Immune Responses in Patients with COVID-19. And the researchers uncovered that hospitalized COVID-19 patients consistently had lower levels of immunomodulatory bacteria coinciding with higher levels of inflammation, and you would think that this would be getting more attention. And what I notice also with the study that kind of jumped out afterwards, and even more so now talking with you, is that they noted that even after they "cleared the virus" their microbes didn't bounce back, it was still at that kind of declined state where they're missing microbes that are associated with robust immune function.
DR. EMERAN MAYER: Yeah. No, this is a very interesting point. It has not received... I mean, this will receive a lot more attention, I'm sure there's... I mean, there's so much research going on in this field that in the next five years we'll see papers coming out on many aspects...
SHAWN STEVENSON: We need it yesterday though.
DR. EMERAN MAYER: Yeah, we... Yeah. So, we've been so absorbed with fighting the pandemic and the vaccine development, which is phenomenal from a scientific standpoint, less so from preventing the next one. And the next one will come. If you see, we've had several smaller ones, but with all the things going on that we've talked about before, the likelihood of these events is increasing, so... Yeah. What is the connections? So COVID-19 enters our body really through the respiratory system, so you're wondering, "What does the gut have to do with it?" 70% of the immune system is in the gut, and a lot of the programming and modulation of the immune system that then goes through all the other organs happens at the gut level. So, the microbes have a big word to say on that. And so, the finding that they reported there could be interpreted in two ways.
One is, if you have a compromised gut microbial system, that by itself will increase the risk that you have exaggerated immune responses to any perturbation, and so it's quite possible that these people that they study they had these abnormalities before they got infected. In this study, they brought in people that were infected and studied them, but in a real longitudinal study, you'd want to know... And these studies are coming out. Somebody who didn't have it and then developed it, did they have this microbial abnormality before that put them at an increased risk?
And I would say that's the more likely because we also know... So, some people get a more severe, got a more severe form of the infection. Some developed this long COVID phenomenon that the symptoms don't go away, and people that are at a higher risk of developing these more severe forms... So, we know who these high-risk populations are. Unfortunately, it breaks down along socioeconomic categories, with socioeconomic in racial... And it's very not genetic, it's probably the correlation of socioeconomic with racial...
SHAWN STEVENSON: Environment.
DR. EMERAN MAYER: Yeah, the environment. So that... Is that a big part of our population eats very unhealthy food, either because it's cheaper or because they don't have access to the Whole Food markets and all these healthy things that are being promoted on the west side of LA, it's not... You go to downtown areas; you don't see the same... So those segments of the population had a much higher risk of not just getting it, but getting a more severe form, and also for this long COVID complication. And we know people that are on this poor diet have a compromised microbial ecosystem, and they're missing exactly those organisms that they've found in these patients, so I think there's a pretty good link between...
It's not just a biological thing. It's also sociological. It's a political thing that... And hopefully, will draw more attention to populations that were most severely affected. And in the jargon of the discussion in the medium, it's always said, "Well, it's the people that have more comorbidities that are more likely to develop the more severe form." Well, what these comorbidities are, as I point out in my book, are the consequence of a unhealthy gut microbiome and over-reactive immune system. So, it all fits together. And I think regardless of where this infection attacks your body, it will always be influenced by what goes in... By your gut health, and indirectly by the things that you feed your gut, your microbes.
SHAWN STEVENSON: Up next in our Microbiome Masterclass Compilation is another one of my truly favorite people, a good friend, Dr. Will Bulsiewicz. He's an award-winning gastroenterologist, New York Times best-selling author of the book, Fiber Fueled, and he's a gut health expert that is really in a league of his own. And he's also the author of more than 20 articles in the top American gastroenterology journals. He's a graduate of Georgetown University School of Medicine and was a chief medical resident at Northwestern Memorial Hospital and Chief Gastroenterology Fellow at the University of North Carolina hospitals. And in this clip, he is going to be sharing with us how our knowledge of the microbiome has changed dramatically just in the last decade or two. Also, what our microbial fingerprint is and what controls it. He's going to share the five types of microbes that reside in and on our bodies, and the foundational connection between your microbiome and your immune system. Just jump into this clip with Dr. Will Bulsiewicz.
DR. WILL BULSIEWICZ: Explosion, explosion of research. This is the hottest, hottest ticket in all of science right now, and it's blowing up everywhere you look. And then the pace is accelerating and hard, frankly, for people to keep up with, which, Shawn, is one of the issues in trying to disseminate this information to people, is that you actually have to put in the time to pay attention to everything that's coming out. It's a lot. So, I mean, you go back to 2006, I graduated medical school from Georgetown in 2006. We knew nothing. We thought at that time that there were literally a couple hundred species that could live within the human and be a part of your microbiome. We thought they were literally a couple hundred species, and the reason why is we didn't really have the ability to test for them, because most of these species, which are bacteria, they won't grow on a culture plate, which is what we've always used to study bacteria, it’s culture plates. So, if the bacteria won't grow, then how are you supposed to study them?
It was around 2006, the year that I graduated medical school, and I'd already, by the way, decided at that point that I wanted to be a gastroenterologist. I wasn't thinking about this. I was thinking about more like, "Hey, I think poop is cool," right? Just to be honest, I'll just be honest, I think poop is cool, and we could talk more about that. But anyway, it was around 2006 that they had this laboratory breakthrough that, for the first time, allowed scientists to get at the microbiome and actually study it. And what they discovered was that, oh my gosh, this is insane. There are literally thousands and thousands of different species inside every single... Basically across the globe, thousands of thousands of different species, and each one of us has our own unique signature, our own unique fingerprint, that is made up of somewhere between hundreds and potentially over a thousand different species of microbes. Shawn, there's no one on the planet that has a microbiome like you, you know?
We could basically assign a fingerprint, a signature to your microbiome, there's no one on the planet that has one like me, and that includes my kids, that includes my parents, and so it's kind of interesting to consider that we are... To pivot towards a slightly different topic, you, and I, if we look at our human genetic code, you and I are 99.9% the same... I mean, clearly, we're not the same person, we look different, we have different interests, they're not exactly the same. We would get along very well. But we are 99.9% the same in terms of our human genetic code, but Shawn, we may be 100% different in terms of our microbes, and so there's this huge variability, and what this gets to is a really important topic in the year 2020, which is bio-individuality. Bio-individuality, and this is the expression of that bio-individuality, which is that we all know I will be the first to admit there is no diet that I can say that will apply to every single human being.
There are rules of engagement, there are rules of biology, but you, me and the people who are listening to us right now are all unique, have unique needs, have a unique microbiome, and because of that, your optimal diet is going to be slightly different, and that's the challenge that we face these days, is trying to figure that out.
SHAWN STEVENSON: Yeah, this is one of the first things when we talked before and why I want to have you on is because of your awareness of that fact, and you being a proponent of that and understanding we're all unique and we all have unique needs. It cannot be this cookie cutter thing, even that my perfect diet that I would want for you, that might not necessarily be the thing that's good for you, or it might be good for you now, it might not be good for you a year from now, and so having that flexibility too, and I love that, it just helps so many more people and helps us to dial in what matters for each of us, but there are some things that are consistent with all of us, and we have these five different types of microorganisms residing within us, so can we cover what those five different types of microorganisms offer everybody?
DR. WILL BULSIEWICZ: Yeah, for sure. Let's take it from the top and let's talk about the microbiome, for those of you who perhaps have only heard a little bit about this topic, which is that our microbiome is referring to the invisible living creatures that are a part of our body that are not human, and they cover us from the top of our head to the tip of our toes, all external structures, all external parts of your body have microbes as a part of it, so that includes your skin, your nose, your mouth, inside a woman's vagina, and here's the weird part, our intestines, because it's a tube that starts at the mouth and ends at the bottom. Our intestines actually face outward, that is where we interact with the outside world, believe it or not. That is actually where we are most exposed, the deepest parts of our body that we describe as our bowels are actually outward-facing, and that is where most of our microbes live. These microbes live mostly inside of our colon which is our large intestine.
And the estimates are that we have about 40 trillion of these microbes. Now to put that into perspective, Shawn, that is more than the number of human cells that you have. You are less than 50% human. More than 50% of your cells come from these microbes, and when we zoom in on these specific types of microbes, it is interesting to think about it this way, but this is a fact. Your gut is an ecosystem, it is an ecosystem in the same way that you would think about the Amazon Rainforest, about the Great Barrier Reef, there is a harmony in balance that exists among the life with the net ecosystem, and it includes these five types of microbes.
So, the main one, are bacteria, that's what you're going to hear us mostly we talk about are bacteria. They are the dominant ones. And we know bacteria. We've heard of E. Coli, salmonella, shigella, but actually it turns out that most of these bacteria are our friends, they're there for a reason, they're trying to help us. Beyond the bacteria, we have fungi, which you could also refer to as yeast. We all have those, like candida is an example of one of those. The third one are the archaea, which are my favorite. Because if you haven't heard of these archaea, let me introduce you real quick. The first life that we detected on this planet was from a dig site in Greenland, it's from four billion years ago, and they were archaea. We believe that archaea are the first life on this planet, and they are hardy, they are resilient. They are not going anywhere.
Global warming can occur, anything could happen. We could have a nuclear war, there was to be archaea on this planet. And you will find them in the bottom of the ocean in a rift vent, you will find them inside of a volcano, and you will find them inside the friendly confines of your colon. And the archaea are part of the balance too. They're not bacteria, they're not yeast, they're their own type of thing, and they're there in a part of the harmony. And then the last two are... You could have parasites, not everyone has parasites, but actually more people have parasites than they would realize, and the last are viruses. Viruses are kind of weird, they're not even alive, they're just basically DNA or RNA structures that can affect and influence how biological processes work. So COVID-19 is not living. It's a virus, and that virus can affect us, and so we have viruses that are a part of us, and they're actually a part of the balance too, they help to maintain the balance within our microbiome.
They're not necessarily problematic or the enemy, they're actually contributing to our health. So that's the lay of the land. Five different microbes creating this ecosystem that's designed, that's really with the engine for human health, this is the engine that makes you healthy. Basically, there is a direct line between the food that you eat and the status of your microbiome. The number one influence on your microbiome is actually your dietary choices, and I actually find that, by the way, to be empowering, because what that means is you're not born with something that you can't change. You have the ability to make your gut microbiome whatever you want it to be, you just have to choose the right stuff to get it there. And so, there is this direct line between the food that you eat and your microbiome.
And then when we zoom in, imagine that we're going in and looking under the microscope, and what you would see inside the colon is that there would be this flourishing community of these microbes, again, the bacteria, the fungi, the archaea, they're all hanging out, and there is this paper-thin barrier called the epithelial layer. This paper-thin barrier is there, it is so thin that is less than the size of a fraction of a human hair, and it's not visible to the naked eye. And on the other side of that paper-thin barrier exists 70% of the immune system, which actually makes sense, because the immune system is meant to defend. And if you were a general, where would you set up your defenses? You would set it up in the place where you are the most vulnerable. Where are we the most vulnerable? Where are we interacting with the outside world? It's there. It's there in the gut.
And so, you find 70% of the immune system there separated by just this single layer of cells, they are literally microns away from each other, and they're communicating. Although they are separate, there is a constant crosstalk, and I described it in my book, and you know this, Shawn, 'cause you read the book, that it's like, I got my house and my neighbor over there has their house, and we got this little dinky fence that separates our house. And when this pandemic is over, I'm going to have a big party. He's going to have a big party, and let's not pretend that those two parties are totally separate, even though there's a fence that separates them, we got our energy, they got their energy, we're feeding off each other, we're talking to each other, we're sharing stuff. And that's the way that it works inside of our gut, is that you literally cannot separate, you literally cannot separate these gut microbes from your immune system.
When I was researching my book, I looked into the connection between the gut and the immune system, and what I found is that all allergic diseases, all autoimmune diseases, where they have studied the health of the gut microbiome, they have discovered in all cases that there is damage to the gut microbiome in people who manifest allergic and autoimmune diseases. The point being, Shawn, that I am of the belief at this point that if you want a healthy immune system, you have to have a healthy gut, and that is the path. And so, if the path to a healthy immune system is through the gut... Well, I just told you before that there's a direct line between the food that you eat and the make-up of your microbiome, so let's talk about and let's focus on our diet, because that is what is going to change your immune system.
SHAWN STEVENSON: Up next in a microbiome masterclass compilation is somebody that you might know, he's a best-selling author of the international bestselling book, Sleep Smarter, and the author of the USA Today national best-selling book, Eat Smarter. It's a clip from yours truly. In this clip, I'm going to be sharing with you a specific way that our microbes influence our body composition, and this is really remarkable, and some specific foods that you can include to support a microbiome that is geared towards a healthier weight. So, let's jump into this clip from the microbiome metabolism master class that I did, and by the way, every single one of these episodes, the complete episode is available for you in the show notes. So, let's jump into our next clip.
As your diversity of microbes goes down, your rate of obesity and insulin resistance goes up. These have an inverse relationship. So, one of the biggest epidemics we're seeing is this decreases, this radical decrease in diversity in microbes, and here's what the impact has on the other side when we improve this. A recent study published in the International Journal of Obesity revealed that a higher diversity of gut bacteria is directly correlated with less weight gain and improved energy metabolism independent of calorie intake. Independent of calorie intake! Calories are not the boss. It's not Tony Danza, it's not the boss. Calories are not Genghis Khan, it's not the emperor, it's not the Mongolian boss, it's not, calories are controlled by other things, namely, one of the most important, is your gut bacteria.
Now, the number one way to increase your microbiome diversity, which is noted in the data, is to increase the diversity of foods that you're eating, that one simple thing. And just think about it, I know for myself, this definitely hit me, how often, even if I'm "eating healthy," how I get stuck in a rut of eating the same things over and over and over again, and all of the different bacteria strains that create the diversity, create overall optimal health, they require different prebiotics, food substrates for them to eat, so that they can proliferate our "probiotics" can actually proliferate, colonize and then create postbiotics. So, the prebiotics enable the probiotics to create the postbiotics, which again is the vitamins, minerals, short-chain fatty acids in you for you that help your metabolism and your health to thrive.
Alright, so we have to give them their preferred food source. In each module, we go through a plethora of specific foods that can transform the health of your microbiome and to support your metabolism. Take blueberries for example, bifidobacteria make SCFAs, make short-chain fatty acids that protect your gut lining and reduce inflammation. Data published in the Journal of Agriculture and Food Chemistry, affirm that eating blueberries increases this bifidobacteria and, listen to this, positively modulates the diversity of gut bacteria overall. Pretty cool. And a study published in the British Journal of Nutrition found that eating some pistachios can also improve your overall ratio of bifidobacteria as well. Real food can do it. Real food. Fake food caused the issue. Real food can help fix it. Alright, so those are just a couple simple, easy things to add in as snacks, or throw some blueberries into a smoothie. Just add them in with your cooking.
There's so many different dynamic ways to get some of these foods in, and these are just a couple. Again, these are coming right out of the pages of Eat Smarter, including this one. A specific SCFA, again, short-chain fatty acid, to support your gut health is propionate, okay? Propionate has been found to reduce inflammation in the gut, and it can help reduce visceral fat. So, this is belly fat. This is a deep, abdominal fat. This SCFA has been proven to help to reduce your ratio of visceral fat. And just to be clear, this is a naturally occurring propionate that's made by your gut flora, and this is not the synthetic propionate that's added to a lot of processed foods that actually increases your risk of visceral adiposity, the growth of visceral fat. So, we want to target real food sources that support your microbes in doing this production of this SCFA. Great sources of prebiotic foods that help you to make propionate are garlic, onions, chicory root, jícama, Jerusalem artichoke, and asparagus.
Those are just some of them. Pretty cool. Pretty cool. Now, another prebiotic microbiome-supportive food that was really surprising to me that's in the pages of Eat Smarter... And this one, again, this one really tripped me out is cocoa, aka cacao, but the powdered... De-fatted powder form of chocolate. A randomized double-blind controlled trial, gold standard of study, published in the American Journal of Clinical Nutrition revealed that polyphenol-rich cocoa has remarkable prebiotic effects in the human body. Study participants consuming a sugar-free cocoa flavanol drink for four weeks significantly increased their ratio of bifidobacteria and lactobacilli populations while significantly decreasing their counts of Clostridia, a class of Firmicutes associated with fat gain. These microbial changes were paralleled by significant reductions in plasma triglycerides, which are blood fats, and inflammation, c-reactive protein concentrations indicating reductions in inflammation. Wow. Shout out to you, chocolate.
Alright, pretty cool. We want to get the best quality we can from the original source of where chocolate comes from, and this is why regularly, again, one of the things that's just on tap here in my household is the chocolate Organifi Gold formula, because it highlights one of these benefits, of course, bringing in this high quality source of cacao and getting the benefits from the chocolate, but also has this incredible combination of other metabolism supportive foods, like turmeric. And turmeric, the active ingredient in there, curcumin, has been found to literally support anti-angiogenesis of adipose tissue, so blocking the nutrient supply of haphazard growth of your fat cells. That's incredible. There are very few foods that we know that are able to have that capacity, and also turmeric is well noted to be one of the most remarkable anti-inflammatory foods ever discovered, so having that in the mix can be helpful as well. So, you get those two major components, all together in one delicious beverage.
So, if you want to get yourself some Organifi Gold, go to organifi.com/model, that's O-R-G-A-N-I-F-I.com/model, and you get 20% off. They're giving you 20% off their Organifi Gold formula and chocolate Gold formula as well. Alright, these are just cool things to add in, they make it easy. The reason that I talk about these things is that I understand the behavior pattern of most of our citizens, and so we're trying to just upgrade, up-level, the things that people are already doing. People are going to drink coffee. They're going to drink it. But what if we can swap that out with a medicinal mushroom-infused organic coffee instead of the pesticide, rodenticide, herbicide laid in frappuccino from Starbucks?
What if we could swap them out? What if we can make them equally delicious without side effects? This is what we're doing now. We've got to up-level, just upgrade the things people are already doing. It makes it an easy on-ramp and easy switch. Alright, so Organifi Gold, go to organifi.com/model, you get 20% off. Alright, so we're going to wrap things up here with two additional points in optimizing your microbiome, and this was another thing that really shocked me. I was by myself in my office when I was writing the book, and this was one of those times I was just like, "Oh my goodness, I can't believe people don't know this." One of the most surprising things regarding diversity and the microbiome is that your gut bacteria can actually change dramatically based on what time of year it is, based on the season. Stanford University researchers discovered that gut microbes and digestion are cyclical and in sync with the seasons and environmental conditions.
So, another tip here to support microbiome diversity and your metabolism overall is to purposefully eat more seasonal foods. And this by no means, again, says that you can't have your favorite foods that might not be in season, but what if we proactively add in some things that nature is trying to signal us to eat right now at this time of year? Because our microbes are cyclical. As we evolved, our microbes would change and adjust as the seasons change. So, these are those things below the surface that can create health from the inside out, so we talked about prebiotics, now, the prebiotics are the food that the friendly flora need, are different bacteria strains need in order for them to proliferate. And we have to understand that the prebiotic foods that we eat are unique to us, if a diet framework has us strip a food away that our ancestors have been eating for centuries, that has been feeding a strain of microbes or strains of microbes that have been protecting you against autoimmunity, protecting you against joint issues, protecting you against inflammation, and now this diet takes it away.
You might even get results with a different calorie management or whatever the diet framework might hold, but then this is why so often folks see diminishing returns as they do the diet. We have to do what's best for us and our unique metabolism. The same thing with, we might start adding in foods that don't necessarily jive with our system, this is why we go through such a diverse array of different foods and stuff that we can experiment with, add in and just have some fun, because the truth is overall increasing the diversity of foods that we bring in, oftentimes, especially if they're real whole foods, they're just going to have more and more benefit.
Next up, we have a clip from a tenured professor of neurobiology at Stanford University, Dr. Andrew Huberman. His laboratory studies neural regeneration, neuroplasticity and brain states, such as stress, focus, fear, and optimal performance. More than 20 years, Dr. Huberman has consistently published original research findings and review articles in the top-level peer review journals, including Nature Cell, Neuron and current biology. And in this clip, he's going to be sharing with you a simple food implement for supporting microbial health plus a shocking way that our microbes might affect our fitness level. So, let's check out this clip from the amazing Dr. Andrew Huberman.
DR. ANDREW HUBERMAN: The two to four servings of fermented food per day, I think one reason I like that recommendation is the signs point to it as beneficial, and also, it's something to do as opposed to something to not do. There's a lot of restrictive practices that are associated with losing weight, et cetera, and those are hard because they're restrictive, but the addition of something that hopefully... I think most people like some form of fermented, low-sugar fermented food. The gut microbiome is so fascinating and it's an area that you can just think of part of you, it's like a little community that talks to the neurons that talk to your brain and really control your appetite. Some people start eating fermented foods and they lose their appetite for really sugary carbohydrate-type foods. They just lose it completely. They just, for whatever reason, they don't crave that stuff anymore, and it's remarkable, but it makes sense. And the microbiome is involved in so many things. I think it's sleep being the fundamental layer of health, and all the light and stuff that goes with it, but I think that the gut microbiome is right up there in the top five or so of critical aspects of our body that we all absolutely need to take care of.
SHAWN STEVENSON: I love that. So, add in some fermented foods. Another thing seen in the data is simply increasing the variety of foods that you're eating. That's another simple intervention that we can do. Because if you think about it, every food that we eat has its own microbiome in a sense. If we eat a blueberry, we're eating that blueberry's microbiome. If we eat an avocado, we're eating that avocado's microbiome. And so, because I think that we have this tendency, and I know that I did earlier on in my career and looking at, again, probiotics, and even prebiotics, and I think that creates this tunnel vision where we might go to Google and find, "Here's the best prebiotic foods." Really, every food functions as a food for something else, for some form of microbes. And so, we know clearly now that having a diversity can help to fortify the diversity of your microbes. As your diversity goes down, your risk of diabetes goes up, your risk of obesity goes up, sleep problems, et cetera. So super simple stuff. Again, we don't have to try to stop doing everything, but just add in a little bit more variety.
DR. ANDREW HUBERMAN: There's even some evidence that... And this is wild and it's just one study, but my friend, Andy Galpin, he is a physiologist and professor at Cal State Long Beach, he's a really skilled muscle physiologist, and he also does the training side, so he knows the stuff under the microscope really well, and he knows the actual practices that a disrupted gut microbiome can actually prevent the adaptive responses to exercise, which is wild. Same caloric intake, same exercise, it's resistance exercise in this case, the muscle adaptation does not take place in cases of what I call dysbiosis when they're not getting enough variety in the gut microbiome.
So, the gut microbiome is foundational. I think that we can talk about it in the context, I mean it's been shown to improve symptoms of autism, there's so many things, cognitive function. It just... It's a fundamental layer. I would say sleep is the fundamental layer, and then gut microbiome is right there in the foundation. And if you want to use the house analogy or building analogy, if the foundation is shaky, nothing else is going to work well, everything else is going to seem harder, the electrical is going to go out, it's just unstable. So, sleep and microbiome are two of the major pillars. They're not the only pillars, but they're two of the major pillars. And what's cool about getting good sleep and taking some control of the microbiome is it makes the other stuff that we're told to do easier, like making the choice to exercise, making the choice to make better food choices, making the choice to have some self-control with respect to the phone use, etcetera.
SHAWN STEVENSON: I hope that you're enjoying our microbiome masterclass compilation. For our final clip, we're going to circle back to one of our experts, but this is a different conversation that I had with the incredible Dr. Steven Gundry. And the reason that I'm putting him in here twice is that he, for me personally, has been the person when it comes to the gut, when it comes to the microbiome, he's dropped the biggest knowledge bombs on me. He's been so far ahead of the curve, it's just remarkable. And so, in this clip, he's going to be sharing with us the interesting similarity between the soil and our microbiome, so again, a similarity between the two and how the modern American microbiome differs from a more traditional hunter-gatherer's microbiome, which is pretty shocking. And also, he's going to talk about the newly discovered communication through gas exchange, taking place in the microbiome. So let's dive into this clip from the amazing Dr. Steven Gundry.
DR. STEVEN GUNDRY: One of the things that I've been fascinated with is, the more I've studied plants, the more I've been impressed that we are basically a plant that carries its soil around with it. So, plants have roots that go into soil, and that soil is actually a complex living system of its own microbiome and its own set of nutrients. And one of the things that's been clear is we've totally destroyed the soil that plants live in. We've used biocides, herbicides, insecticides, we've mono-cropped, and so our soil is actually dead. So even though a plant may look like a plant, maybe a leaf of spinach looks like a leaf of spinach, it's nothing like that spinach of 50 years ago.
In fact, the US Senate in 1936, 1936, almost 100 years ago, said, "Our soil is now so depleted of nutrients that we could eat continuously and never get the nutrients we need to sustain a healthy life." 90 years ago, they knew this, and one of the theories of all this is we are seeking out nutrients, and we keep eating until we get those nutrients. And one of the interesting theories of obesity is, guess what, you can eat and eat and eat, and we are nutrient depleted in all of our food sources, and you'll never get them. The second thing that's really exciting is, speaking of the gut, it turns out our gut is the same surface area, the lining of our gut, as a tennis court. And the reason it has such a surface area, 'cause everybody looks down at their gut and say, "There's no tennis court down there," is we actually have roots. We have a shag carpet on the inside of our gut, and these roots are called microvilli, and they literally are similar to the roots of a plant. And the soil of us is actually our microbiome, those trillions and trillions of bacteria and fungi and worms, and the food we make basically compost, if you will, and our roots go into that soil, and we're turning everyone into a great gardener, and if we take care of our soil and take care of our roots, we will actually increase our ability to extract energy from the food we eat.
SHAWN STEVENSON: We want to be healthy, robust plants, not necessarily Little Shop of Horrors.
DR. STEVEN GUNDRY: Exactly, no. "Feed me, Seymour."
SHAWN STEVENSON: So, this gets into the conversation, and I love that analogy, by the way, of we really are plants that have gotten up and walking around, and we've taken the soil with us. But I've said the statement many times, and I talk about this in my book as well, that chronic nutrient deficiency leads to chronic overeating, period.
DR. STEVEN GUNDRY: Yeah.
SHAWN STEVENSON: We have this innate drive through our evolution to seek out nutrients to help our bodies to run processes. Very simple principle, but the more we're eating deficient foods, we might get some substance in our body for a time, but those mechanisms that are calling out for copper, for boron, for magnesium.
DR. STEVEN GUNDRY: Magnesium, yeah.
SHAWN STEVENSON: Yeah, they're just going to be going off continuously until we get our needs met. And you mentioning that 90 years ago, saying this soil is already just devastated, and where we are today, oh my goodness.
DR. STEVEN GUNDRY: Yeah, as I mentioned in the book, this is the US Senate document, it starts one of my chapters. And I actually, when I address physician groups, I actually put the slide up of this quote from the Senate, but I don't put the date, and I ask them, "Guess when this quote from the Senate was," and people say, "Oh, 2000," or "Oh, 1980," and then I flash up 1936 and people go, "What?" We've known this long that we've had this problem, and no one's done anything about it.
SHAWN STEVENSON: Yeah, until now. We got to make the change.
DR. STEVEN GUNDRY: Until now. Now we're going to get the roots and soil back to normal.
SHAWN STEVENSON: That's right, I love it.
DR. STEVEN GUNDRY: You and I will do it. Come on.
SHAWN STEVENSON: Just me and you, hand-in-hand. You know what, this, again, this really gets into the conversation for me of like, what does it look like when we have a robust healthy root system and soil internally? And we know what that looks like based on the data from folks who are eating closer to more of an indigenous diet...
DR. STEVEN GUNDRY: Exactly.
SHAWN STEVENSON: Which you talk about as well.
DR. STEVEN GUNDRY: Yeah, this was one of the real eye-openers. I knew about this study long ago. The Hadzas in Tanzania are one of the last surviving hunter-gatherers that really stick to their traditional culture. And the men go off hunting every day, they walk eight to 10 miles. The women gather berries and tubers, and they walk on average, three to four miles a day, and they're very thin and very fit. So researchers said, "Gee, let's look at the energy expenditure of these people and compare them to the modern office worker," and I bet you're going to find, because these guys are lean and fit and they're walking all over the place, that these guys are lean and fit 'cause they're burning through energy and they're just energy-consuming, whereas the desk workers, they're sitting there, sitting on their ass all day, and what they found just shocked them. The energy expenditure of the Hadzas was exactly the same as a desk worker. And you go, "What? How can that be?" Well, in research, we have to make a conclusion, otherwise, we won't publish our paper. So, these guys said, "Well, the reason for that is that everyone's got a set amount of energy expenditure, and it's universal across the board." And I went, "What? No." What's happening with these desk workers who clearly aren't producing energy by moving, they're using up their energy with this fire of inflammation, and all their extra energy is being consumed in this fire. And it's...
I mean, it's just the most amazing thing that we had missed, that obvious point. Energy was being produced and consumed, but it was being consumed or rather being used to do things, like walk eight miles.
SHAWN STEVENSON: Right. Man, the human body is just amazing and resilient. Now, what about the microbiome of these folks versus the average person in the western world?
DR. STEVEN GUNDRY: I am glad you asked. So, these guys, we'll use them as an example, they vary their diet seasonally. During the summer, which is their dry season, they hunt and eat wild animals. During the wet season, they actually eat a lot of berries and actually consume a lot of honey. And their microbiome changes dramatically from season to season. And the number of species in their microbiome is very, very diverse. It's moving, it's organic, it's like a tropical rain forest, all these different species. You compare that to us, any western diet, and we have a very non-diverse microbiome, we have very few species, and it never changes. And what we think is important is that those species do need to change on a circadian rhythm basis, on a seasonal basis, to actually tell our mitochondria how to produce energy. And this is probably one of the most startling discoveries in the book, and if I may talk about postbiotics.
SHAWN STEVENSON: Yes, please, please do.
DR. STEVEN GUNDRY: Okay. So, everybody... Postbiotic? What that heck is a postbiotic? So, everybody knows probiotics. These are the friendly bacteria. And you eat your yogurt to get your probiotics. Or you eat your sauerkraut to get your probiotics. Prebiotics are the fibers that friendly bacteria have to eat to, number one, stay alive, and number two, to produce chemical messengers that are called postbiotics, that actually tell mitochondria, their sisters in all of our cells, whether to make a lot of energy or whether to throttle back on energy production. And the discovery of this communication system actually won the Nobel Prize for medicine in 1998, but it's only recently been discovered that there is a language between the microbiome and us, our genes, our cells, that is primarily gases. Like for instance, fun fact, hydrogen gas, so everybody farts, and everybody seems to be embarrassed by farting, but I actually tell readers to step on the gas, because the more gases that people make by eating prebiotics, the more you actually tell your mitochondria to produce more energy.
SHAWN STEVENSON: Whoa. That... When I... I literally highlighted this because you talked about how bodily gases are important for our mitochondrial function...
DR. STEVEN GUNDRY: Yeah.
SHAWN STEVENSON: And neurotransmitter function and hormone signaling, and you labeled these gasotransmitters.
DR. STEVEN GUNDRY: Yeah, they're called gasotransmitters or gasomessengers, but it's actually now described as transkingdom communication. So, the kingdom of bacteria and the kingdom of fungi actually talk to the animal kingdom, and even the plant kingdom, through gases. We knew that there was somehow an exchange of information, but we didn't know what it was. And literally, the discovery of these things is as important as the discovery of the Enigma code in World War II where we broke the German language code in World War II, and it was called Enigma. And this discovery just opens up so many possibilities. Let me give you hydrogen as an example. So, we know from work in Japan that people with Parkinson's Disease and neurodegenerative disease don't have a microbiome that produces hydrogen gas, and people who don't have Parkinson's have a microbiome that produce hydrogen gas. So, you give people with Parkinson's disease hydrogen water, which is hydrogen dissolved in water. They get better as hydrogen... They can absorb hydrogen by drinking it. They get better by replacing hydrogen.
Even something as rotten as hydrogen sulfide, the rotten egg smell, turns out to be incredibly beneficial for telling mitochondria to make energy, number one, and actually give them a substrate to make energy. And it's probably really good for your brain function as well. So, who knew that... In some cultures, it's actually a sign of respect for the chef to break wind at the table.
SHAWN STEVENSON: I bet everybody didn't think we'd be talking about farting today. But it's so funny that this is one of those taboo things... Of course, I'm thinking about the scene from Nutty Professor where the family's like talking through farts at the table, but...
DR. STEVEN GUNDRY: From Blazing Saddles.
SHAWN STEVENSON: Right. It's a classic. So, I think that there's going to be a conflict, this image of, what about gas and bloating? What about IBS? These things versus the healthy performance of gases in our body, which is actually essential.
DR. STEVEN GUNDRY: Yeah, that's a great question. And I see a large number of patients with IBS and complaints of gas and bloating, and many of them have tried the FODMAP diet, for example, or the specific carbohydrate diet to eliminate this problem, and I assure my patients, number one, that if you want good mitochondrial health, and if you want good energy production, these diets are the exact opposite of what you want for long-term good health, because you have absolutely starved the most important part of your body of the things they need to eat the microbiome. But what we do is we stepwise re-introduce little bits of these prebiotics, and the whole book is a stepwise introduction of new habits, and this is one of them, a stepwise way. And once you do this, you begin to tolerate those gases, and you get a perfect balance between too little is really bad, too much is really bad, but we want to hit the Goldilocks rule of just right, and that's what we get people to do.
SHAWN STEVENSON: Alright, thank you so much for tuning into this compilation, this Microbiome Master Class compilation. I hope that you got a lot of value out of this. If you did, please share this out with your friends and family on social media. Of course, you can tag me, I'm @shawnmodel on Instagram and on Twitter, and I'm @TheModelHealthShow on Facebook. And of course, you can actually send this right from the podcast app that you're listening or watching on, and let people know to check out this episode ASAP. We've got some powerful master classes and incredible guests coming your way very soon, so make sure to stay tuned. Take care, have an amazing day, and I'll talk with you soon.
And for more after the show, make sure to head over to themodelhealthshow.com. That's where you can find all of the show notes, you could find transcriptions, videos for each episode, and if you got a comment, you can leave me a comment there as well. And please make sure to head over to iTunes and leave us a rating to let everybody know that the show is awesome, and I appreciate that so much. And take care. I promise to keep giving you more powerful, empowering, great content to help you transform your life. Thanks for tuning in.
Maximize Your Energy
Get the Free Checklist: “5 Keys That Could Radically Improve Your Energy Levels and Quality of Life”
HEALTHY MEALS EVERYONE WILL LOVE
The Greatest Gift You Can Give Your Family is Health
When you gather your family around the table to share nutritious food, you’re not only spending quality time with them - you’re setting them up for success in all areas of their lives.
The Eat Smarter Family Cookbook is filled with 100 delicious recipes, plus the latest science to support the mental, physical and social health of your loved ones.













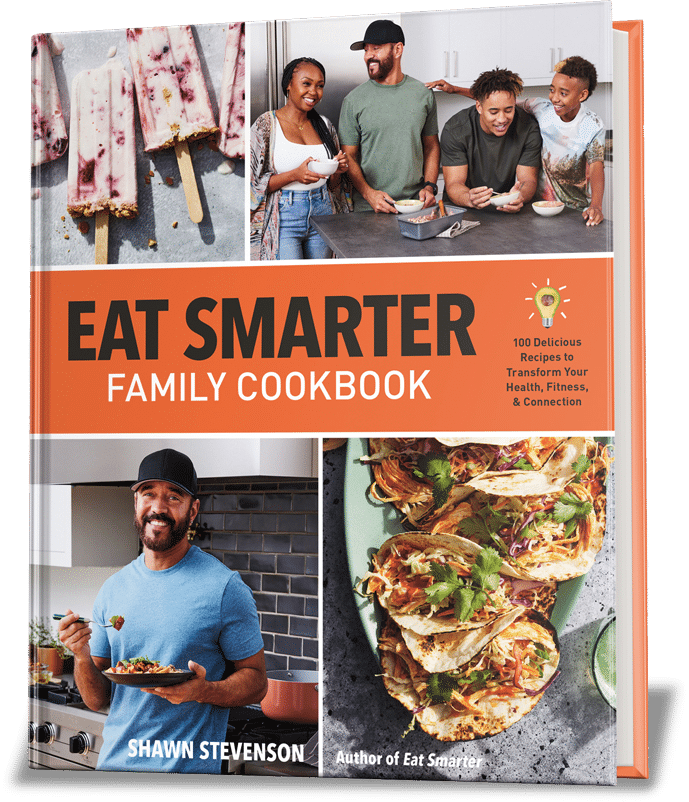
Share Your Voice
0 comments. Be the first to leave a comment.