Subscribe to The Model Health Show:

TMHS 694: The Truth About Obesity
In the US, rising rates of obesity have become a public health crisis, and epidemic, and a threat to our collective health and quality of life. Despite this knowledge, rates of obesity continue to climb, and most popular solutions leave much to be desired in terms of long-term efficacy. On today’s show, we’re going to dive into the truth about obesity.
We’re going to talk about the science of fat cells, how they work, and the role of inflammation in obesity. You’re going to learn what’s behind surging obesity rates, and the connection between obesity and the leading causes of death. This episode also contains science-backed information about popular prescription weight loss drugs, and alternative, proven therapies for treating obesity.
This episode will arm you with key information on human health, immunometabolism, inflammation, and a whole lot more. Part of the solution to the obesity epidemic entails empowerment and education, and that’s what you’re going to hear today. I hope you enjoy this episode on the science of obesity!
In this episode you’ll discover:
- The ten leading causes of death in the US, and their relationship with obesity.
- How many US citizens are overweight or obese.
- What the number one risk factor is for death from COVID-19.
- The science of immunometabolism.
- How obesity impacts immunosurveillance.
- The role of body fat in the endocrine system.
- How your body fat controls your metabolism.
- Different types of fat communities in the body, and their roles.
- How storage fats can accumulate toxicants and forever chemicals.
- The connection between body fat and inflammation.
- Why understanding epigenetics is the key to treating obesity.
- How financial consequences drive treatments for diabetes.
- What GLP-1 is, and its role in satiety.
- The connection between GLP-1 agonist drugs and thyroid cancer.
- Specific foods that can help modulate GLP-1.
- How olive oil consumption can aid in fat loss.
- The importance of reducing brain inflammation in improving body mass.
- Three simple, proven treatments for obesity.
Items mentioned in this episode include:
- Organifi.com/Model — Use the coupon code MODEL for 20% off!
- Onnit.com/model — Save an exclusive 10% on performance supplements & tools!
- The Calorie Myth with Jonathan Bailor – Episode 10
- The Shocking Truth About Drug Companies with Dr. John Abramson – Episode 552
- Eat Smarter
Thank you so much for checking out this episode of The Model Health Show. If you haven’t done so already, please take a minute and leave a quick rating and review of the show on Apple Podcast by clicking on the link below. It will help us to keep delivering life-changing information for you every week!
Transcript:
Shawn Stevenson: Welcome to The Model Health Show. This is fitness and nutrition expert Shawn Stevenson, and I'm so grateful for you tuning in today on this episode We're going to be doing a special deconstruction of our obesity epidemic what's really going on behind it? What are some of the numbers really looking like and also what are some of the new treatments that have been brought forth recently, in particular some new medications, in addressing obesity, how effective are they? So, this is going to be an incredibly enlightening episode, packed with science, so really tune in and pay close attention. So first and foremost, you want to understand something, why does this matter right now? Well, obesity is the primary risk factor for all 10 of the 10 leading causes of death in the United States. Let's take cancer for example. According to the NIH and The National Cancer Institute, obesity and being notably overweight significantly increases the risk of at least 13 types of cancer. This includes a higher risk of colon cancer, breast cancer, pancreatic cancer, and a two times higher risk of liver cancer, a two times higher risk of kidney cancer, and a four to seven times higher risk of endometrial cancer, or uterine cancer.
Now in addition, again, this is according to the NIH, obesity and being notably overweight significantly increase the risk of heart disease, stroke, liver disease, kidney disease, arthritis, and more. And a study featured by the NIH and published in the International Journal of Epidemiology followed study participants for 11 years and found that obesity substantially increases the risk of dementia, stating, "The study found that the association between obesity and dementia was independent of whether a person was a smoker, had hypertension or diabetes, or carried the APOE4 gene, which is a genetic risk factor for Alzheimer's disease and related dementias. So, they looked at all the confounding factors because you cannot prove causation in a study like this, a longitudinal study, but they're going to do their best to remove potential confounding factors that might disrupt or influence the data. So, despite whether the person was a smoker or not, whether they had hypertension or diabetes, two huge risk factors for developing dementia, and whether or not they had the gene that's most strongly correlated, again correlated not causative, of dementia, whether or not they had this gene, being obese or significantly overweight was one of the primary risk factors for the development of dementia.
Now again, I want to reiterate this point that our obesity epidemic as a society right now, we're knocking on the door, somewhere around 250 million United States citizens are now overweight or obese. Alright, so we're talking about the vast majority of our population. Something is awry, something serious is going on here. And to tie this to our top 10 leading causes of death, we're not talking about vanity metrics. We're not talking about shaming anyone. We're talking about science and how we can protect ourselves and create a new path to wellness for our families, for our communities.
But for us to do that, we've got to actually understand what we're dealing with. We've got to take a good look at the problem. And if you're curious, like what are those 10 leading causes of death? So, this is according to the CDC and some of their latest numbers for 2021. Number one is heart disease, the champion of all causes of death for many, many years here in the US. Heart disease is number one, cancer number two. And with heart disease, we're talking around 700,000 deaths, cancer not too far behind with about 605,000 deaths. Then we have the age of COVID-19 coming in at number three as of 2021. Number four is accidents, number five is stroke, Number six is chronic lower respiratory diseases. Seven, Alzheimer's disease. Eight, diabetes. Nine, chronic liver disease and cirrhosis. And 10, kidney disease and related conditions. Now some of these might stand out like, wait a minute, what does obesity have to do with this particular condition?
Well, let's dig in and talk about this. When you hear COVID-19, you might think like, what does obesity have to do with COVID-19 really? Like is this backed by science? Well, a huge analysis that was conducted by the CDC, published by the CDC in July of 2021. The researchers looked at over 540,000 COVID-19 patients from over 800 US hospitals. And they determined that obesity is the number one risk factor for death from COVID-19. The number one risk factor for death from this condition, this infectious disease that really took over our reality, globally, right? So the number one risk factor, right? But again, oftentimes that's pushed to the side. Are we blaming obesity for the problems and the fallout from COVID? And the framing gets twisted instead of just acknowledging like, this is the number one risk factor. Maybe we can do something to insulate ourselves, our families and our communities from future issues that would arise. Because again, we're seeing a new age of infectious diseases. Like we thought earlier, 1970s, 1980s, that we kind of had infectious diseases in check. We had through Better Living, through chemistry and science really gotten a handle on these things. But they've continued to grow precipitously. And we've got many things, obviously, that are probably going to be coming down the pipeline, so wouldn't this be a good time for us to address a primary risk factor for poor outcomes from infectious diseases.
Now, what about accidents? Accidents are on the top 10 leading causes of death in the United States. That seems strange that obesity might be tied to something like that. Well, this is something that I've had my eye on for a little while now, and there are a couple of really important studies I want to share with you. One of them was published by Johns Hopkins, Bloomberg School of Public Health, and they tracked the BMI, The Body Mass Index of nearly 8,000 workers from eight different manufacturing plants, and analyzed the distribution and prevalence of workplace injuries. The researchers found that 85% of all injuries occurred in workers who were overweight or obese. With clinically obese workers having the highest rate of injuries overall. As BMI was increasing, accident risk increased right in combination with it. So as BMI trends up in the data, accident risk trends up right along with it.
For instance, those who were categorized as severely obese with a BMI of greater than 40, had the most injuries to the hands, wrists, and fingers. So, hands, wrists, and fingers. And that was about 22% of the people. So, for instance, those who were categorized as severely obese with a BMI of greater than 40 had the most injuries to the hands, wrists, and fingers when compared to the same injuries occurring in other weight categories. Now again, this should not be a means of discrimination. This should be a means of education and support for workers and citizens of all classes to have a level of empowerment and a sense of sovereignty within their bodies, and an ability through education and through choices to better protect themselves from injuries, from chronic diseases, and to be able to maintain their health.
And that's what it's really about. But again, we can't solve a problem we don't understand. We can't address this issue if we don't know that it exists. And even more interesting in this domain of accidents being a leading risk factor of death and how obesity ties into it, even things like car accidents, an analysis published in the Peer-reviewed Journal, frontiers titled Aging Obesity and Motor Vehicle Collisions found that obese occupants, drivers and/or passengers had a 54% to 61% higher risk of injury compared to normal weight occupants. Alright? The question is, what's going on here? What's happening behind the scenes that would decrease our resilience when we are faced with a trauma, a stressor, an environmental insult? And we're going to dig into that a little bit more, but again, I want you to understand some of the research and understand that this is not just hearsay, these are science backed determinations, and to really light a fire under us to start to do something about this.
Now, another one in that category of the top 10 causes of death in the United States was respiratory infections being a leading killer every year without interruption. This keeps showing up as a leading cause of death. And the question is, why? What's going on in relationship to obesity that could be creating more of a vulnerability towards respiratory infections, things like the common flu and colds and other infectious diseases? What's going on here? What happens with our bodies and our immune system and this susceptibility? Well, there's an entire field of science looking at something called immunometabolism. Alright. Immunometabolism. This speaks to a couple of things. One is the metabolism of the immune cells themselves. Our immune cells, like all of our cells, have a metabolism, alright?
They're consuming things, they're processing things, they're eliminating waste and they're replicating. And certain things from our environment, our choices, our exposures influence how efficient and intelligent our immune cells metabolism is working. So, we've got that one flavor of immunometabolism, but also how the metabolism or the health of the overall being, the overall person is influencing the out-picturing or the functionality of our immune system as well. So, what's happening there? How can our immune system, our immunometabolism be disrupted if we're struggling with obesity?
Well, one of the things that happens is a depression of something called immunosurveillance. When we venture into being overweight or obese, we have increased dysfunction in something called immunosurveillance. So, this is essentially our immune system's capability of identifying pathogens and threats to our system, right? So not really being on top of things that we're exposed to. Number two, venturing into a state of obesity and faced with infectious disease like a respiratory illness, for example. When we have a higher rate of obesity, we have increased systemic inflammation. So, inflammation is controlled and guided by our immune system itself. So, we're already in a pre-inflamed state as the excessive energy that's getting put into our fat cells. As its expanding, it's sending out somewhat of a false distress signal to our immune system as if we're infected. And so, we already have a heightened state of inflammation, and then we get hit with something, an infectious disease, or a pathogen, and that can exacerbate inflammation more. And thus, we see this kind of trickle-down effect of poor outcomes.
Another issue here when we venture into a state of obesity that makes us more susceptible to respiratory infections is that obesity disrupts immunomodulation. So, this is our immune system's ability to make an accurate or an appropriate response to a pathogen, right? Maybe heightening its response, right? So, being hyperactive for a stent or bringing our immune response downsome, if our immune system is overactive right? A quote cytokine storm is taking place, or if we're talking about something like an autoimmune condition, helping the immune system to intelligently tamper down. And another issue here is an increase in the onset of immunosenescence. So, when we are battling with obesity, we're battling with carrying excess body weight, we are going to see a acceleration take place, an acceleration take place of the death of our immune cells right? None of this sounds good, but these are all things that are taking place.
Again, this is not about vanity. This is not about trying to look good. This is about being in a state where we are resilient and healthy, and we can enjoy our lives our livelihoods. We can help to dramatically reduce the risk of death from all manner of conditions. Because again, data from... People want to cite the NIH and the CDC in regard to one flavor of things, new drugs that come on the scene. Everything's referring back to them. Are people really looking at this data because they're saying the number one risk factor for this infectious disease that has just kind of taken over our lives the past few years, the number one risk factor is obesity. That's from their data, right? And also tying in how obesity is a major contributor to the 10 things that kill the majority of our citizens.
Are we going to do something about this or are we going to deflect? Are we going to explain this away? Are we going to try to treat this like it's some kind of superficial thing? Are we going to treat this like we can find a magic pill or a magic drug to help to eliminate this system? So again, we're just getting the ball rolling to really unpack what's going on behind the scenes. But most importantly, again, I want to point our attention to the fact that what's happening is we're losing a remarkable amount of resiliency when we're dealing with so much excessive weight that we're carrying. We're going to see a lack of function or dysfunction with our cells, our tissues, our organs, and our organ systems. Alright...
There is going to be a tremendous amount of inherit stress excessive stress that we are carrying that we are trying to operate and get by, but this speaks to also the resilience of the human body overall, to be able to carry that and to still be able to show up and do what we have to do. But what if we can make it easier for ourselves? What if we can stack conditions in our favor so that health, both metabolic health and mental health, becomes the norm? I know this is possible. And again, this starts with education and understanding truly what's going on behind the scenes. "We cannot solve a problem from the same level of thinking that created the problem" to cite Albert Einstein. Now, if we're talking about obesity, we tend to put our focus onto body fat. Now, yes, this is obviously a big player in this, but again, we're trying to target something we don't really understand. So, let's dive in a little bit more and talk about our body fat and how it works, because again, we're trying to get rid of something that we don't understand or villainizing something that we don't understand without any real context.
Now, our body fat is an organ. Alright we tend to think that our body fat is just these scattered droplets of unhappiness that are just around our body somewhere, but it's actually a coherent organ that's communicating throughout your body with lightning speed all the time. And more specifically, it's an endocrine organ. You know what that means? Do you know what an endocrine organ means? This means that it's a hormone producing organ. It's producing a plethora of hormones. Now, here's the thing. Here's one of the rubs. Some of the primary hormones that body fat's going to be producing is going to be excessive amounts of estrogen. Estrogen is not bad. Estrogen is beautiful. We all need estrogen. Thank goodness for estrogen. It enables so much from the function of our cognition to our regulation of our metabolism, the health of our thyroid, obviously reproduction.
There's so many important facets of estrogen boosts. Like with so many things in life, an overabundance of one thing can damage the system. And so, when we are growing excessive amounts of body fat, we're pumping out increasingly high amounts of estrogen. Now, body fat releases, hormones and other substances that help to regulate our metabolism by communicating with other organs and tissues such as your liver, your pancreas, and your muscles. Now, this introduces a critical but overlooked point that your body fat is itself a controller of your metabolism, right? Your body fat itself is a controller of your metabolism. So, the health of your body fat, the state of your body fat is inherently going to control what's happening with your metabolism. This is not about some micromanagement of one energy substrate. We label something as a calorie, for example. This is bypassing the understanding of things that have this epi-caloric control that is controlling what calories are doing in your body. And your body fat itself is controlling what calories are doing in your body.
Now keep in mind, there isn't just one flavor of fat. There are a variety of different fat cell communities that we've been able to identify in recent years, and different fat cell communities are responsible for different things. We have structural fats, like the fats that enable the function of our brain and our nervous system. And we have fats that play significant roles in thermogenesis like our brown adipose tissue. And we also have highly specified storage fats. Right? Storage fats. Now, this is the type of fat that we tend to think about when we are targeting "fat loss". We're trying to target our storage fats. The key player in your storage fat community is the fat cell itself. You want to think about this being a citizen who's a part of something bigger, right? So just like with anything here on planet Earth, we are still, all of it still existing in this giant, glorified snow globe, alright? We're not separate from the thing. We might have this individuality, but we're a part of the whole. And the individual fat cell itself is the key player in fat storage. And fat cells have an uncanny ability to store energy.
This is an incredible evolutionary advantage and adaptation that made humans stick around. We made it. We made it here. Alright. AI might have something to say about it, but we made it here. Alright. And a big reason is our ability to, again, without us thinking about it and micromanaging calories through our evolution, our body has been able to store energy and utilize it during times of famine, and to also have really intelligent systems to eliminate excess. Alright. Our fat cells are incredibly intelligent. Our metabolism is incredibly intelligent, but the template that we have as a human right now is not hardwired for the conditions that we live in today. Even just 100 years ago, 20 years ago, just a couple centuries ago, life was radically different. We did not have this 24/7 excessive access to all manner of caloric density. So again just to use that label, because it's far more complex than just the calories, but we just have so much excess right now that we're just swimming in. And also couple that with so many different innovations that remove physical activity from our livelihood. There are less and less things that we need to do to move to be able to do it. And we start to create a recipe for destruction here. And with that said, how good are these fat cells at storing energy? How good are they? Damn, is he funny? Sorry. That's from, Def Comedy Jam. Shout out to Joe Torry, St. Louis's own just like me.
Now, how good are they? Fat cells are able to expand their volume more than 1000 times their normal size. It's crazy. It's crazy what our fat cells are able to adapt to and to do for us. It's able to carry that, it's able to take a plate home, not just take a plate home, but take a whole smorgasbord, take the whole freezer, take everything home with you, and to keep it for when you need it. And that's really the point I want to keep bringing us back to, because our bodies are very intelligent at storing energy for a rainy day. But in our society today, that rainy day never comes. Alright. So, it's not that our body is trying to punish us by storing energy. It's what it does. It's what it does. These storage fats, store energy. If you give us in abundance, that's what it's going to do. That's what it's designed to do. Now, our fat cells, which are also referred to as lipids or adipocytes, are mainly comprised of tiny packets of stored triglycerides. Now, triglycerides, we've got Tris. We've got a three of something. We got glycerides. Alright. So, we've got essentially three fatty acid molecules attached to a single glycerol molecule, triglycerides. And what's crucial to understand here is that our fat cells literally, again, join together in different communities that work towards certain functions or getting certain things done.
So, our storage fat community works together cohesively to do its job of storing energy until instructed with very specific messaging to let that energy go. Alright, let my people go. Alright. Now, just to reiterate this point once more, is that what's happening when our body fat grows is that our fat cells themselves are growing. We're generally not having new body fat cells being produced or created. And there is a place where that happens, and we've talked about that on previous episodes. And there's also, of course, there's going to be a process of replication. There's going to be a process of cellular senescence where our fat cells are dying off, but then they're getting replaced. But there are certain occurrences where our body can start to make more fat cells. But in general, what we're seeing when we have excessive accumulation of body fat, we're seeing that the body fat cells themselves have grown in size. Now, as mentioned, our body fat cells are storing excess energy, from the things that we've consumed. But here's where it gets really interesting. Fat cells are not just packed with triglycerides. They're also used as growable storage depots for things like persistent organic pollutants.
This category of forever chemicals and other toxicants. According to a study published in the peer-reviewed journal, Comprehensive Physiology, the lipophilic nature of newly invented environmental chemicals leads to the bioaccumulation of them in our fat tissue. The scientists indicate that many of these newly invented toxicants are lipophilic, lipo meaning fat and philic, meaning loving. Alright. So fat loving.
Alright, you might be fat loving in some ways, and that's okay. Alright, or you might just be McLovin, shout out to Superbad. But this denotes that these compounds are drawn to bind with body fat. Now, the researchers are demonstrating that when we gain excessive weight, we become a magnet for these environmental toxins. The researchers noted that PCBs, PBBs and other industrial chemicals are incredibly resistant to biodegradation. And these compounds readily find a home in our fat cells as our body fat levels expand. The scientists stated, "bioaccumulation in expanded adipose tissue mass of obese subjects can exert inflammatory actions that could contribute to the development of insulin resistance and low level persistent organic pollutant exposures may contribute to the development of diabetes and other inflammatory related conditions".
Who's telling us this? Who's telling us that just living in this world right now, living in this environment, this modern environment is causing us to gain weight. Is causing us to develop diabetes. Is causing at its core, dramatic cellular dysfunction. We're exposed to things that our tissues they're finding a way to adapt and to protect us from these things. And so, tucking them away in our fat cells which again, they evolved to protect us. They evolved to help keep us alive. But now we just want to get rid of it. We want to do whatever we can to get rid of it. We don't understand its purpose. We don't understand what it's trying to do.
And again, if we're not addressing the root cause of why we're in this situation, we are never going to find a solution. And we're very likely going to be the victims of profiteering as we're getting sold all manner of things that are newly invented along with these environmental pollutants that are not removing the root cause of why this is happening. An incredibly concerning issue with this today is that there's an estimated 10 million new chemical compounds unleashed into our environment every single year. A recent study published in the journal, Frontiers in Ecology and the Environment states the research community is falling woefully behind in studying the chemicals, pesticides, pharmaceuticals, and other novel concoctions discharging into our air, our oceans, waterways, soil, and food chain. The truth is conventional science has no idea what all of this new chemical exposure is doing to us. They have no idea. They're not studying it. There's too much. There's so, again, the research is woefully behind, woe, woefully behind.
It's insane. And again, we're experiencing all of this exposure and this stressor, this newly invented stressor, newly invented stressors. A plethora of millions of these things. And most people have no idea. And we get into the situation where we are beating ourselves up and we're trying so hard to make these changes not realizing that things are stacked against us. Now, is this the only issue contributing to obesity? Of course not. Of course not. But does it add more fuel to the fire? Absolutely. Because also, these things are coming along with our largely ultra-processed food diet. According to the BMJ, about 60% of the average American's diet is now ultra-processed foods. When you hear ultra in front of it, this isn't just normal, minimal processing that we evolved having with food, taking olives, and making olive oil, for example.
This is taking corn and through newly invented ways of processing, high heat extraction, through the addition of added flavors and colors and stabilizers and environmental pollutants inherently happening all over this process, we get on the other end that corn combined with not just the corn itself, high fructose corn syrup or whatever relegated sweeteners is going into this mix. We get something like Pops cereal. Alright, we get something like Lucky Charms out the other end. That's an ultra-processed food. You can't tell if somebody came, who's living in a hunter-gatherer tribe and then they come here and they see a box of Lucky Charms. They have no clue at all where it comes from. We don't. And we live here. We eat that sh*t. We don't know where it comes from. We just know that the guy on the commercial says, "what's at the end of the rainbow? I got you. Come get some of this."
I don't know if you've seen the Leprechaun horror movie by the way, if you haven't seen it, don't see it because it's crazy. And I think Leprechaun 4... It is crazy how these movies keep getting made, they got sequels and... Who's out here checking for a Leprechaun? Alright, but I think part four is Leprechaun in the hood. Alright, so nevermind. Alright, now, again, we lose touch with reality 'cause that's what happens when we're eating ultra-processed foods. We're losing touch with where that food actually came from. It's no longer food. It's a food-like product. It has the appearance of something that you can eat. It's edible, but it is so chemicalized and denatured. Your cells cannot possibly associate with this stuff and have a positive health outcome, alright.
This is not to say you can't eat a bowl of Lucky Charms every now and then if you're feeling lucky, alright. It's not about that. It's about, in particular, understanding, okay, in reality, when I eat this, yes, it is a significant stressor to my body. It is going to cause some issues with my...
My pancreas, my insulin, my heart... I'm feeding myself this stuff. It's not real and it is what it is. I'm choosing to do this because most of the other stuff that I do is really good for me. This is a totally different situation, but I don't want us to lie to ourselves and act like this is cool, this is food. It's not. Now to circle this back to what this conversation is really about, which is really understanding this multi-pronged epidemic of obesity. Another huge factor in this obesity equation is the role of inflammation and how it disorients the normal function of our fat cells and our brain as well. So, I mentioned with our fat cells, inflammation is going to be heightened because our fat cells are themselves going to be sending out a distress signal, inciting the response of our immune system.
This is why we see higher rates of systemic inflammation once we venture into being overweight and into obesity. But the brain equation is a major player in all of this, and scientists at the Albert Einstein College of Medicine reported that hypothalamic inflammation, so inflammation in our hypothalamus, which is regarded in many scientific circles as a master gland or the master gland in the human body regulating things like thermogenesis, our body temperature, regulating our nutrient expenditure, regulating our sleep, influence our heart rate. The list goes on and on. Truly important. But they reported that hypothalamic inflammation is a double edge sword in nutritional diseases. The study authors reported that systemic inflammation from things like metabolic dysfunction and carrying excess body fat leads to higher rates of brain inflammation. And brain inflammation itself leads to metabolic dysfunction and excess body fat. So again, it becomes this vicious circle once we incite inflammation in our brain, in particular with the hypothalamus.
So, and we might be like, "well, how do I know if my brain is inflamed?" If we're carrying excessive amounts of body fat, there is a high probability that our brain, in particular, our hypothalamus is trying to deal with all of this and there's going to be inflammation that's taking place, and that inflammation can then spur about more body fat. But there's good news we can help to put this fire out potentially. But this is going to take a multi-pronged approach because obesity isn't the result of just one thing. But recently there was a news segment on 60 Minutes, very popular show, it's been around for a long, long time, that is essentially pointing to one major causative factor of obesity. And I thought that we would unpack this conversation a little bit to provide some context and to really provide some enlightenment, because shows like that reach a lot of people, obviously.
But here's the thing, shows like this potentially, oftentimes reach more people. And so, getting right education to counteract education that might be a little bit shortsighted is incredibly helpful today. Because what tends to happen in nature is that a problem is presented, and a solution is presented as well. And so, in this first segment that I'm going to share with you, the researcher... A leading obesity researcher is going to be sharing some valid science regarding changes in the brain when people develop obesity, making it more difficult to keep weight off once someone loses weight through conventional methods. Here's that portion of the segment.
Dr. Fatima Cody Stanford: It's a brain disease and the brain tells us how much to eat and how much to store.
Dr. Fatima Cody Stanford, an obesity doctor at Mass General Hospital, an associate professor at Harvard Medical School says, common beliefs about obesity are all wrong.
It is your turn to get on that scale.
And diet shows like the Biggest Loser...
You lost 128 pounds.
Are snookering people. If you diet you lose weight, right?
Dr. Fatima Cody Stanford: For many of us, we can go on a diet, something like the Biggest Loser. You go and you restrict people. You make them work out for 10 hours a day, and then you feed them 500 calories. For most people, they will acutely lose weight, but 96% of those participants in the biggest Loser regained their weight because their brain worked well, was supposed to bring them back to store what they needed or what the brain thinks it needs. So will power. Throw that out the window. My last patient that I saw today was a young woman who's 39, who struggles with severe obesity. She's been working out five to six times a week.
Now, in that segment, she talked about how the body adapts its set point and this set point theory, which is going to be new for a lot of people, especially people that are watching that show. But do you know when we talked about setpoint theory the first time on the Model Health Show? 10 years ago, a decade ago, episode 10, with Jonathan Bailor, New York Times bestselling author, science researcher, we talked about setpoint theory then. The thing is, we're talking about something that is inherent within the human operating system. Within really all species, there's going to be a set point. Yes. However, that doesn't stop us from doing things that socially and as a system of healthcare that are unethical and pushing people to do things that are not effective in the long term because they're not addressing...
An intelligent way to modulate our set point. For example, referencing the Biggest Loser Show as was in that segment, Jonathan Bailor at the time, 10 years ago, was working with some of the participants from The Biggest Loser after the show who had this dramatic increase in their weight. And they were suffering so much because they were trying so hard to keep that weight off. But being on that television show with this abhorrent amount of exercise and dieting, and it's really strange because we're watching this take place. We're spectators in this basically fat sport and cheering on the Biggest Loser. Even the title itself, it's a double entendre, but looking at it in the other way, like who the... The person that's the biggest loser, not the loser of weight, but overall, how could that even be pitched as a thing?
And I've actually been pitched and invited to participate in many of these weight loss shows over the years, and I've declined every time because it's so highly unethical from my perspective. Now, the key here in her statement about weight gain is that this weight loss is through conventional methods that don't intelligently healthfully reestablish a new set point. Yeah. Conventional methods don't work. Clearly what most people are told to do, this cookie cutter caloric management burn more calories than you take in. Yes. Lack of education around all the things that we cover here on the show. Yes. But despite her citing something valid when talking about set point and the influence on the brain, when it comes to weight loss, suddenly things took a turn for the worse.
I've always heard that it's the fast food that it's the Diet Cokes, that kind of thing. That is the instigator. Is that true?
Dr. Fatima Cody Stanford: So, I think we have to look at the different cause of obesity as a big pie, and that's one factor. But notice how I'm using this part of the pie, right? But the number one cause of obesity is genetics. That means if you are born to parents that have obesity, you have a 50 to 85% likelihood of having the disease yourself. Even with optimal diet, exercise, sleep management, stress management.
Now here's the thing. This well-intentioned researcher and scientist is sharing with a large public viewership that their struggles with obesity are due to genetics. Right? It's not your fault. This is largely due to genetics. Now, again, I'm sure that she intends well, but where are we at with science today? Well, in an analysis that was published in PLOS One, the Public Library of Science one, one of our most prestigious medical journals titled Genetic Factors Are Not the Major causes of chronic Diseases, demonstrates that genetic testing is also... Right. We got all this genetic testing defined the cause of diseases. The researchers uncover that genetic testing is also rapidly affirming, that supposed genetic risk factors are not actually causing a, our numerous epidemics of chronic diseases, including obesity. When it comes to obesity, we've been able to identify some genes that are correlated with obesity, but there has never been a gene discovered that causes obesity. That doesn't exist.
Just like we talked about earlier in the scope of dementia, one of the primary, the APOE4 gene, that is again correlated with dementia. There is a significant sect of people in the study that we talked about earlier who didn't have that gene and yet they had dementia. And the same thing holds true here. Yes, we know about certain genes that are correlated with obesity, but today the leading science is epigenetics. Epigenetics, epi meaning above genetic control, above genetic control. Our genes are just blueprints regardless if it's for an expression of creating and maintaining more body fat, we also have the ability for those genes to essentially get muted. And for the expression of other genes that would be more robust towards the utilization of stored body fat. We all have all of them because we all came from ancestors who survived in times of feasts and famine.
Our genetics don't just change in the last 40 to 50 years when we've seen this skyrocketing epidemic of obesity. It's not the genes that changed, it's the environment that changed. Genes don't work like that. We don't just suddenly, that takes time. Genetic adaptations and mutations take time. And we're talking on the scope of like thousands of years. This is not going to change in a couple of decades that suddenly the genes are doing the thing. Because if that was the case, this would've been around for a long time, not just a couple of decades. This genetic theory that is the primary causative agent of obesity, there would've been when we had access to more, even if it was minimally processed food like we did in the earlier part of the century, we would've seen an acceleration in obesity regardless as she's downplaying the role of what we're eating. Right? So, keep this in mind, but the report goes on to share this.
In one of her published studies, Dr. Stanford found that most medical schools don't teach that obesity is a disease, and in fact don't even offer courses on it even though it's the second leading cause of preventable death in the country after smoking.
Now, here's where the message gets really incongruent, because if obesity is the second leading cause of preventable death after smoking, their assessment is incredibly bizarre. Because if it's primarily genetic, how is it suddenly so preventable if it's the second leading cause of preventable death. That's like conflicting, it's oxymoron. Emphasis on the moron in that statement, right? So, it's immediately downplaying the fact that this is largely preventable if we're talking about this condition. Now, if death from smoking is a number one preventable cause of death, people need not to smoke to avoid it, right? If death from obesity is a second leading cause of preventable death, what do people need not do in order to avoid it? If genetics is the primary cause, should they avoid things that activate those particular genes? Haha Haha. A haa.
But wait, there's more. There's no way this segment on this prestigious show could be an advertisement for the new obesity drug, could it?
Dr. Caroline Apovian, co-director of the Weight Management and Wellness Center at Brigham and Women's Hospital in Boston.
Exercise is good. I'm walking a lot.
Who sees both Maya Cohen and Nicole Sams is relieved that at last, she has a highly effective medication to offer her patients that's safe according to the FDA.
Dr. Caroline Apovian: What the medication does?
It's part of a new generation of medications that brings about an impressive average loss of 15 to 22% of a person's weight and it helps keep it off.
Dr. Fatima Cody Stanford: A major issue were...
Doctors Apovian and Stanford have been advising companies developing drugs for obesity, including the Danish company, Novo Nordisk, an advertiser on this broadcast.
She said it, the new obesity drug being an advertiser on that broadcast. Crazy. Crazy pants. It's right in your face. We're not hiding it. It is what it is. And after that portion of the segment, they slide right past the concerning side effects and the lack of data approving its, data proving its effectiveness for a long-term weight loss. And the other featured physician, Caroline Apovian, Dr. Caroline Apovian, is featured and talks about the stigma around obesity being the reason she can't give this drug to all the patients that she wants to.
Dr. Caroline Apovian: That's where the stigma of obesity comes in. The idea that the patient can do it with diet and exercise. You would never do that to a patient with hypertension or heart disease or type 2 diabetes. Tell them that "you just don't eat sugar, you'll be fine."
Novo Nordisk also makes a drug for type 2 diabetes called Ozempic, which most insurers and employers do cover. What frustrates the doctors is that Ozempic and Wegovy are exactly the same drug, though Wegovy for obesity is usually prescribed at a higher dosage.
Now, there's two major issues here when she's talking about this stigma. Number one, she's comparing people who receive drugs for hypertension and type 2 diabetes to the people who are being deprived of drugs to treat their obesity. But that doesn't make any of it right, effective or ethical? According to the Journal of the American Medical Association, hypertension and type 2 diabetes are predominantly caused by poor diet, sedentary behavior, and other lifestyle factors. Prescribing a costly drug to treat the symptoms that manifests from those behaviors is not removing the cause of the thing, it's just extending the suffering. That's what it really is doing, and it's creating a cash cow out of the individual. Again, at is its core, because in truth, we're treating a symptom. We're trying to mute some of the body's biological feedback from exposures and choices and environments that are causing dysfunction and harm within the body.
Muting that signal does not remove the cause. This is why so many people who are prescribed, for example, a statin, end up developing another condition like the study that was published in the BMJ titled Statin Use and Risk of Developing Diabetes, looking at patients being prescribed and using statins to reduce their risk of cardiovascular disease, having an increased incidence of developing diabetes. The causative agent being this abnormal, intrusive element coming in as a blunt instrument, trying to disrupt the pathway of cholesterol being created in the body. What other things is that going to influence? It's going to influence the function of the pancreas. It's going to influence the function of our insulin sensitivity, our leptin sensitivity, the function of our liver. The list goes on and on.
Nothing is operating in a vacuum in our bodies. But again, trying to treat a symptom with a blunt instrument is probably going to have "side effects", but it's not really a side effect, it's a direct effect. So to say, we give drugs to everyone else who has lifestyle related diseases. Why are we not giving more drugs to people who have obesity? It's incredibly unethical because it's not actually treating the root cause of any of these conditions. Disease symptoms are persisting in the body and now they're very likely going to have additional disease symptoms from habitual prescription drug use. And the patient is milked for their money and their life force is very likely going to die from the very disease that they were given drugs for. That's the truth. It's happening every minute, every day right now.
Now the second major issue when she's talking about this supposed stigma is that this 60 minute segment is a glorified pitch to one, get viewers excited about a drug that's effectively a magic pill that you can take to lose weight without proactively changing your lifestyle. And two, the segment is an appeal to insurance companies to cover the drug, which they inevitably will so that all parties involved can make more profits. And it's all under the guise that it's really about protecting people. But if they really cared about that, they would appeal to insurance companies to cover science backed lifestyle interventions prescribed by our healthcare practitioners like this randomized controlled trial pitting lifestyle changes up against conventional drugs for the treatment and prevention of diabetes as shared in a conversation we had with Harvard professor, Dr. John Abramson.
Dr. John Abramson: So that's the diabetes prevention study funded by the NIH, National Institutes of Health, not by the drug companies. And it's a very well-designed study because it wasn't just a drug against placebo to see if we can prevent diabetes. It was a drug against placebo against lifestyle to see what the best way to prevent diabetes is not what the best drug to prevent diabetes is, but the best way to prevent diabetes and the clear winner was lifestyle intervention. And that is a stunning result. Not just because it shows that lifestyle is superior to medication, which is superior to nothing in terms of preventing pre-diabetics from going on to get diabetes. But the really revolutionary finding in that study that has not sunk into doctors consciousness is that you can get people to make lifestyle changes. This is a randomized controlled trial. They didn't cherry pick, they didn't take people who were willing to exercise.
Dr. John Abramson: These are randomly assigned people. People are randomly assigned to the groups. And the people who were randomly assigned to the intensive lifestyle counseling lost about 10 pounds and kept it off and were exercising about five times a week and continued to. So, you can do this and the epidemic of diabetes, which you described exactly correctly, Shawn is clearly an epidemic, a consequence of the epidemic of obesity in American society. 40% of American adults are obese now. It's going to be 50% within about 10 years. And this is just purely a consequence of our lifestyle, of what we're eating and how much exercise we're getting. And somewhat modified by socioeconomic circumstances because people who are less wealthy have less opportunity to make the voluntary choices to get out of this lifestyle. So, we don't want to be discriminatory here. Some people really can't avoid it, but most of us can.
And what we're doing, the problem is, and this is the whole problem with our approach to healthcare, this is it in a nutshell. The problem is that the drug companies can make money with the downstream treatment of people who get diabetes, but they can't make any money. There's no big companies with major swaths of shareholders that are going to make money by Americans going to eating healthy diets and getting proper exercise and otherwise living healthy lifestyles. Nobody's going to make big money doing that. And the real underlying problem, of what we're talking about is the way the financial consequences drive the epistemology. What we believe to be true about these diseases is driven by the financial consequences, not by the medical and health and well-being consequences.
SHAWN STEVENSON: Just to share this directly from your book, so we had a placebo group. We had a one group that was given Metformin, and then we had the lifestyle intervention group. And the group who received the Metformin had a 39% improvement in their results in reducing the risk of developing diabetes, which is notable, 39%. But the folks who received the lifestyle intervention and coaching had a 58% reduction in their risk, almost 60%. Like it's unbelievable. The ultimate takeaway that I want folks to take, because there's a lot of healthcare practitioners who listen to this show, is that we want to stop with the excuse making and get better at our jobs of educating and supporting folks because it is...
Dr. John Abramson: Absolutely.
SHAWN STEVENSON: It is absolutely possible. And also, it's probable, once we get the right information in people's hands, give them basic support and the resources, as you mentioned they exist. It's just what are we doing with it? And so, one other little interesting point, and this really came out for me as I was reading like never before. It really, really struck me. And I don't know if a lot of people ever even think about this. A lot of scientists ever think, never think about this. And this is a game changer. If we're looking at the effectiveness of a drug, we're usually looking at the effectiveness of a drug versus nothing.
It's... The gold standard of study, a randomized placebo-controlled trial is having the drug go up against nothing. It's not going up against another drug, it's not going up against a lifestyle intervention. It's not going up against a well-documented, proven supplement. It's going up against nothing. And so is nothing better than something or is something better than nothing. That's really the argument that's taken place, taking place. And, in our science in our healthcare system is built upon that premise. And it's not right when we have, again, mountains of peer reviewed evidence on the efficacy of basic things that our genes expect from us, like movement, like real food, these essential things. Not to say that drugs cannot be supportive in these tenets, but if we're not getting the essential stuff, we're window dressing.
Dr. John Abramson: That's exactly right, Shawn.
SHAWN STEVENSON: Now here's the thing. These newly invented drugs that are said to target obesity, Ozempic, Mounjaro, Wegovy, and there are others in this category, the framing is that these drugs target a specific hormone, a satiety related hormone called GLP-1, and is as if targeting this hormone in isolation is going to do the job. The reality is that it's going to alter the function of every other cell and, in the human body with this synthetic drug. The primary side effect appears to be mild to severe nausea. Why? Why is this the primary side effect? Well, GLP-1, Glucagon-like peptide 1 is a hormone produced primarily in your gut. When nutrients enter your intestines, it's a signal that your body is bringing on a certain nutrient and getting things stored. GLP-1 has been found to increase the feeling of fullness during and between meals by acting on the appetite centers in your brain and by slowing the emptying of your stomach itself. GLP also through these means influences our blood sugar levels as well. Now targeting areas of your brain, like the hypothalamus that controls things like your heart rate, body temperature, etcetera.
Ooh, well, where we're fiddling with the brain with this newly invented synthetic thing, is this okay? And also keep in mind that the hypothalamus is part of the HPA axis, this information superhighway that's controlling so much of your endocrine system. And do you know what's along the HPA axis as well? Your thyroid. Really considered the master regulator of your metabolism. And one of the more concerning issues with this new class of obesity drugs, as stated by the Mayo Clinic, "Ozempic and other formulations like Wegovy, has been associated with an increased risk of thyroid cancer." How? Why would that... Oh, the HPA axis. According to their own drug data, "Ozempic has caused thyroid cancer in animals. It's unclear if this drug also increases thyroid cancer in humans." Unclear Sounds like a red flag to me.
Lab animals are going to develop, mice are going to develop the cancer much more rapidly, their lifespan. It's just one of those things. Cancer development, for it to be detectable in humans, it takes years. It's... It's all hot, it's all... It's all good right now. Got Americans shooting up Ozempic and its buddies. But what are the long-term ramifications? There's actually a black box warning on Ozempic from the FDA. It states that in rodents Ozempic, "Causes dose-dependent and treatment duration dependent thyroid tumors." Dose-dependent, how much are you taking? Duration-dependent, this means the longer you're taking, it keeps increasing that risk of thyroid tumors. This is po... It's positioned from these healthcare practitioners to be something; you get on it and you stay on it. But it's fine. It's fine. She'll be alright.
Now again, this is under the guise of targeting GLP-1, which is valid in its roles in helping to support metabolic health and satiety. But we don't need a drug to do that. As a matter of fact, there are a plethora of safe, long-studied ethical ways of managing and modulating GLP-1 without these severe, potentially fatal side effects that we're going... Again, this is the beginning. This is the beginning. You know where this train is going. Let me give you some of the examples. A fascinating study published in the journal, Gut, looked at a compound called propionate that's found in a prebiotic fiber called inulin, and it was shown to significantly increase the release of GLP-1 and other satiety hormones as well. Where do you find this mythical inulin? Asparagus, artichokes, leaks, garlic, to name a few. And isn't it kind of interesting that inulin sounds a lot like insulin? Maybe it's good for managing that too. And actually, the words have the exact same spelling. The only difference is an S, Shawn Stevenson.
Okay. So, what's also really interesting is that chlorophyll has been found to increase the release of GLP-1 as well. So, this is the green hue that you see in plants. This is the blood of plants. So green... Anything that has this green hue in the plant kingdom, you can identify that it's going to be a source of chlorophyll as well. And again, chlorophyll has been found to increase the release of GLP-1, which according to research published in the Journal of Endocrinology, Journal of Endocrinology, big time publication, it has the potential to trigger body fat redistribution. Chlorophyll can trigger the release of GLP-1 and incite body fat redistribution. This literally means that eating foods that are rich in chlorophyll could spark the decreases of visceral fat and a healthy increase of subcutaneous fat. Visceral fat is that belly fat, organ fat around the midsection that is much more noted as a risk factor for those leading causes of death that we've been addressing throughout this episode.
Alright. So, the subcutaneous fat is much safer and appears to be more protective against metabolic diseases. So GLP-1, through getting some chlorophyll-rich foods in, can help this body fat redistribution. It's pretty cool. Now, the question might arise, what if I don't have time to get these chlorophyll-rich foods in? It's just too hard. It's hard out here for a pep. What if? What if? What if? Should I just get my Mounjaro and shoot up or should I just get my Ozempic shoot up? Pause. I got you. Listen, it's never been easier at any time in human history to access these things. You've got a choice here between a synthetic, newly invented drug or foods and this category of "super foods" that have been around for thousands of years that have mountains of peer-reviewed data. If we're talking about the comparison of side effects here, it's not even in the same stratosphere. Food first. Something that your cells can more readily identify with and associate with getting that access. My oldest son, as I was leaving out today, this is something that's just built into his regimen, if...
You know, if he knows that he might be not eating the best quality foods, he really even ramps it up. But every day is built into my family dynamic. Our kids are utilizing things like green juice from Organifi, and it has some of the most chlorophyll dense superfoods ever discovered. Chlorella, for example, it's even gotten its name derived from its rich chlorophyll content. And spirulina, spirulina is also 70% protein by weight. Chlorella is 50% protein by weight. Some of the only places ever discovered that has compounds like phycocyanin. This is like an ancient nutrient that is one of the few things ever discovered to trigger stem cell genesis, like the creation of new stem cells, which stem cells help to regenerate any tissue that might be damaged. Ozempic can't do that sh*t. Let's be honest about this. If we want to buy something, if we want to utilize something to target GLP-1, let's do something that's safe and proven first. Let's do something that employs a habit change where I'm actually proactively improving my nutrition intake. Because as I'm rattling off these different nutrients, one of the richest sources of magnesium is going to be found in Spirulina and chlorella. You're going to find beta carotene, zeaxanthin, lutein. I can go on and on with the antioxidants. Protective, protective versus the other.
So again, if you want to invest in something, invest in real foods first and foremost. And if you want a supplement, get real food concentrates. And that's why we mess with companies like Organifi. That's why they're a part of our family dynamic. These are things that are on our counter, in our cabinets, because they're based on earth-grown nutrients and real foods, real food concentrates, and it's all organic. So if we're talking about these environmental toxicants and all the things, what do you think's coming along with these synthetic drugs? I mean, come on. That being said, Organifi's green juice is definitely a go-to for us, and it's 20% off. You get exclusive 20% off by going to Organifi.com/model, that's O-R-G-A-N-I-F-I.com/model, you get 20% off all of their incredible superfood concentrates and in particular, green juice might be the go-to in particular for trying to target GLP-1, other satiety-related hormones. A lot of people actually, that's part of the feedback. If you even look at some of the reviews, just like it incites more of a feeling of satiety and fullness like, "that's really interesting," this is just basic biochemistry. Now to take this a step further and something that's really practical for targeting GLP-1. A recent study published in the journal nutrients had study participants to replace some of their dietary carbohydrates with some avocado instead.
The participants saw an improvement in their blood sugar levels, reduced levels of the hunger hormone ghrelin in higher levels of the satiety hormones PYY and GLP-1. GLP-1. Thank you avocado. With, and again that's objective measurement using the scientific method and overall, subjectively the participants reported higher levels of satisfaction and reduced hunger for longer periods of time. That wrinkly fruits out there doing this thing if we want to have a tryst with it. So many wonderful ways that we can do this in a way that is efficacious, that's safe, that's smart. It's just what kind of information are we getting fed? Now since we're on GLP-1, we're going to keep riding this bad boy all the way out. Another study, this was published in the Journal of Research and Medical Sciences, and it put participants on matching reduced calorie diets for three months, with one interesting difference, one group included almonds in their diet while the other group did not. After the data was compiled the folks who included almonds in their diet lost twice as much weight and had a greater reduction in their hip to waist ratio than those in the almond-free group. The researchers found a greater improvement in insulin sensitivity and the satiety hormone GLP-1 in the almond group. Almonds. Almonds.
Almond joy. Almond joy got them nuts. Alright? Come on now. We're talking about real almond joy here. Now where are these studies coming from by the way? Where where can I find these so gracefully compiled? Well, I'm reading these studies directly from my USA Today National Bestselling book, Eat Smarter. Alright. So, this information, GLP-1, I've been on it. I've been on that. Alright. And you could be on it too. Now, another study, this was published in the journal Appetite, uncovered that compounds found in green leafy vegetables like spinach and kale were able to significantly increase post-meal levels of GLP-1 in study participants. And this corresponded with a greater reduction in weight, body fat, and waist circumference over the course of the 12-week study period. I'm feeling like Captain America right now. I could do this all day. Alright, but I'll just one more. One more. A recent study published in the American Journal of Clinical Nutrition found that consuming olive oil a little more than a tablespoon triggered the release of not one, but three of our body's major satiety hormones associated with enhanced fat loss. And in particular, test subjects who were instructed to include olive oil with their meals had significant increases in GLP-1, CCK, which reduces overall appetite as well, and PYY, which has been found to decrease the likelihood of body fat storage.
Olive oil. It's been around a long time. Who knew olive oil incites the release of GLP-1 that we're trying to do with these drugs, right? And cultures, long-lived cultures that utilize olive oil are radically healthier than our population here in the United States that the primary oil we're taking in is often highly processed olive oil, minimally processed, low temperature. That's what the virgin part means. Okay, low temperature-processed, cold pressed versus the incredible high heat. The bleaching agents, the deodorizing agents, and more that goes into "vegetable oils, canola oils, and the like." That's the primary oil we're finding in our foods today. In particular, ultra-processed foods, which it's ultra-processed oil. Swap those oils out, change your oils, get your oil changed, can have some incredible benefits for our metabolism. Now, just like so many of the other chronic diseases that are literally killing millions of our citizens every single year, just like many of these other chronic diseases, the drugs that have been created to treat them have not actually brought about a resolution, they haven't brought about a cure to heart disease, a cure to cancer, a cure to diabetes.
The list goes on and on and on. What we're doing again, is buying into a system that has become masterful in treating symptoms and neglecting even the education around root causes of diseases and treatments that remove those root causes of diseases. And just like with this obesity issue that we are dealing with as a society; this problem is not going to be solved with a magical drug. That's not how reality works. It just doesn't work like that. And it's not addressing, again, the root cause of obesity in any form or fashion. Now, earlier in the episode I shared that obesity is shown to create a four to seven times higher risk of endometrial cancer, cancer of the uterus. Well, I have a family member who's been obese for several decades who was recently diagnosed with endometrial cancer. And she went in for the first portion of the conventional treatment, which was to remove all of her reproductive organs to get rid of the cancer.
And so, within that context of that surgery, that procedure is the inspection, like to make sure that we quote, "got it all," and to monitor, measure, see if there's an escape route that the cancer could have taken. And so, a couple weeks after the recovery process, and now devoting herself to a healthier lifestyle, she goes in for a follow-up and her physician recommends that after doing some analysis, seeing that there's some swollen lymph nodes, that she now embark on chemotherapy and radiation just in case. And when I was asking her about, "So where is the cancer located now? If we're talking about chemotherapy and radiation, where is the cancer at? What type of cancer is this now? What are we dealing with here? Can you provide me some context?" And she's going through her paperwork and just can't seem to answer the question.
I was just like, "Wouldn't it be a good idea to know what you're actually dealing with here before embarking on this particular treatment?" And so fortunately, she was able to, the day that she was scheduled to start the chemotherapy, to put me on the phone with her physician. And so, she called me, it was on speaker, and I had a conversation with her oncologist. And the first thing that I asked him about was just like, you know, and of course I'm being very cordial and very curious, and I was just like, "You know what? She can't seem to explain to me what cancer you've detected. Like where is this cancer? What type of cancer are we dealing with here?" And he said, well, actually, "You know, we got some swollen lymph nodes here. It could be from the surgery, but we're not sure."
And so just as a precaution, we decided that this would be the... It's a standard of care to do this. And he did mention that there was some antigens related to cancer that were elevated. But here's the thing, prior to the surgery, they were substantially higher, and they had dropped by over 50% already. And so, I mentioned that to him and I said, "this is a substantial drop from what it was." And he was like, "Well, it's not necessarily substantial." And I was like, "What? That's a over 50% reduction. That's a clinically relevant amount, is it not?" He's like, well, then he changed the subject. And so, she doesn't have any detectable cancer. They've not confirmed it. Even, it's 2023. We have the means to determine if somebody has cancer or not. But he didn't do that because this is just standard of care. Now, that was my first question. My next question was asking if he could help me to identify what was the probable cause of this endometrial cancer that she's dealing with? And he suddenly responded in a very breezy way that, "We don't really know, but it's very likely that this is due to genetics."
And when he said that I knew that she felt that, "Oh, it's my genes. This hasn't... It just happens. It's nothing to do with me, it's just my genes." But here's the problem. He didn't run a gene panel on her. He didn't analyze any of her genes. He just said that sh*t and is so inappropriate. But it's just textbook things that he's going to do to create a sense of trust in him and a trust in the process regardless of evidence. And again, he relented to blame genetics instead of giving me a viable answer like, "What is the cause of this? Where does this cancer come from?" Like if she doesn't remove the cause, wouldn't the cancer come back despite the treatment if the cause is still there? Well, you know, there's going to be a reduction in...
He did not once acknowledge her obesity. He did not acknowledge that she's been smoking for almost 50 years. He did not acknowledge the fact that she's been extremely sedentary for decades, drinking soda for decades, having a significant portion of her diet being ultra-processed food for decades. He did not acknowledge the abhorrent amount of stress and trauma that she's lived through. He didn't mention none of that sh*t. "It's her genes. It's her genes." It's the fault of her genes, even though he didn't look at her genes. So, my final question was, "Just for her mental health so that she can feel more certain in this decision, I would love if you can give me a proposed risk reduction from this procedure. Like what is her potential life expectancy with this procedure after five years? And please give me the absolute risk reduction, not the relative risk reduction."
And even posing this, I know he doesn't know. I know, I'm hoping, of course, if he's not an adamant researcher, if he doesn't have also in conjunction with an MD, also a PhD, he's probably not even aware of the difference of a relative risk reduction, clinically relevant number. Essentially comparing one trial or portion of a trial to another versus the absolute risk reduction, which is what is your risk reduction as an individual in the real world? And I said, "If you've got to just send the data over to me, you could just email it to me." He's like, "No, no, no, no, no, no, no. I've been doing this for 25 years. I know, I know, I know my numbers." He said it was a 65% risk reduction in death in the next five years. And I knew that was the relative risk reduction, which is not the number that I was asking for because I looked the number up with her procedure and just to get a ballpark idea...
It was somewhere in the ballpark of 5% risk reduction of death at the most over the course of the next five years. Now, to make my point more valid, I asked him, "Well, it would be so helpful for her mental health if you could just share some case studies of patients that you've treated with this protocol who are past that five-year mark. And it would just really be helpful to share those case studies. Maybe even if she could talk to somebody who's gone through the treatment, who's survived past that point." He said, "Actually, I've got a patient who's actually doing her last treatment today, who had a more aggressive form of cancer. She would love to talk to her." I was like, "No, no, no, not today. Not somebody in the treatment today, somebody that has survived for five years." And he said, "Oh." He started laughing. He said, "Oh, I'd have to look into my clinic back in Montana. This is in Missouri, by the way, back in Montana. And I have to really rack my memory files to...
He can't give one example of somebody who's alive. 25 years, he said he's been doing this thing, 25 years he can't give me one person. I got all kinds of case studies and examples. You named the condition, the people that we've successfully helped who's alive today. So many stories. He didn't have one, red flag, but I got the red flag, she didn't. When I asked afterwards, because the one good thing that came out of it is that he offered up to getting a second opinion. And he did that because he was flustered. He was just like, "I know, like something is off here in this conversation, my articulation of this thing." And so, she was able to get her ass out of there. And I asked her, "Did anything come off as strange or like did any red flags?" The one thing that she remembered was that getting the chemotherapy and radiation was going to increase her chance of survival by 65%.
The number was not even relevant to her as an individual in the real world. And he didn't have one person to affirm that stat that he could share. But that's what's jumped out to her. For other people it's going to be the genetics. You have to be versed in this stuff. Like so many people are going in disempowered without basic education about these procedures, about these drugs, and understanding truly the risk involved. There's such a lack of informed consent about these procedures, about these drugs. Going back to the black box warning on Ozempic used to treat obesity, one of the hottest things on streets. Black box warning from the FDA on the drug itself, states, again, in rodents, "Causes dose dependent and treatment duration dependent thyroid tumors." And so, in summary, I want you to be empowered, and I want to make sure that you understand that we are not dealing with a vanity issue here in the society.
I want everybody to love themselves, to love the body that they're in, and to appreciate how our bodies have carried us through all manner of challenges and joys in our lives. We need to love our way into better health, not hate ourselves and not shun each other, but in reality, when it boils down to it, we are dealing with a very severe and deadly issue, and we have to get this education into more people's hands. Just to rattle off a couple of reasons why obesity is such a primary culprit in cancer development. And this, again, this is directly from the NIH and the National Cancer Institute.
Here they shared a couple. And if you're watching the YouTube version, you'll see these things on screen. A couple of mechanisms that explain why obesity increases the risk of cancer. One, fat tissue produces excessive amounts of estrogen. High levels of which are connected to risk of breast cancer, endometrial cancer, ovarian cancer, and other cancers. They also stated people with obesity have increased blood levels of insulin and insulin-like growth factor. High levels of these are known to be a cancer risk factor.
In particular, high levels of them promote the development of colon cancer, kidney cancer, prostate cancer, and endometrial cancers. People with obesity often have chronic inflammatory condition that are causative of oxidative stress which leads to DNA damage and increases the risk of cancers. Fat cells also produce hormones called adipokines that can stimulate or inhibit cell growth. For example, the level of an adipokine called leptin in the blood increases with increasing body fat levels. And high levels of leptin can promote aberrant cell proliferation. While another adipokine, adiponectin is less abundant in people with obesity than in people with a healthy weight, it may contribute to an anti-proliferative effect that protects our bodies against tumor growth.
There are several other issues noted but one other possible mechanism in this is obesity could impair tumor immunity and changes the mechanical properties of the scaffolding tissue that surrounds developing tumors. Again, so we can do masterclasses on all of these things. This is a very real, very prevalent phenomenon in our culture. And most people have no idea what's happening inside of their bodies. And this is why this education matters and you being the model matters. And of course, sharing this information with the people that you care about.
And in closing, I want to share with you three simple, impactful, proven, if we're talking about evidence-based treatments for obesity, these are a couple of principles to follow. Number one, it's not the calories alone but the substance those calories come from that can make all the difference in the world. A study that was published in the journal, Food and Nutrition Research, had test subjects to consume a meal of processed foods or a meal of whole foods. And they were both sandwiches but one of them had whole grain, lower processed bread, and cheddar cheese. Lower processed cheese. While the other had white bread, significantly processed, more processed, ultra-processed. And cheese product, which is akin to Kraft Singles which they cannot legally call it cheese because there's not enough cheese in the cheese.
And so, they use objective monitoring to track the path of those calories that they consumed. Here's the thing, both sandwiches had the exact same amount of calories. Both sandwiches had equal amounts of fats, proteins, and carbohydrates. But after eating the processed food sandwich, the participants had a 50% reduction in calorie expenditure after eating that sandwich. Something happened to clog up their metabolism making their body retain more of those calories that they consumed. It's not just the calories, it's the substance those calories are coming from. Where does this play out in the real world, in a real-world study?
Researchers at St. Louis University sought to discover what happens with fat loss when you eat a high carbohydrate breakfast from ultra-processed food, a bagel versus a high protein/high fat breakfast being eggs from a whole food. When the calorie count of the meals is the exact same. The researchers did have study participants decrease their overall caloric intake by a thousand calories a day but had different people use different macronutrient ratios for their first meal, just their first meal. Here's what happened after an eight-week study period.
The study participants who avoided the processed food, bagel breakfast, and ate eggs instead had a 61% greater reduction in body mass index, a 65% greater weight loss, a 34% greater reduction in waist circumference, and a 16% greater reduction in body fat. This is what's possible. This was in eight weeks. Same calories, whole food, ultra-processed food. High protein food, high carbohydrate food. None of these macronutrients are villains. But what are we starting our days with? So that's number one. It's not the calories alone but the substance those calories come from that make all the difference in the world.
Number two is to keep inflammation in check. We talked about how scientists at Albert Einstein College of Medicine reported that hypothalamic inflammation is a double-edged sword for nutritional diseases, citing how systemic inflammation from things like excess body fat leads to more brain inflammation. And brain inflammation itself leads to more body fat. A primary contributor or reducer of inflammation has to do with the dietary fats that you choose. Because fats are integral in energy utilization by the body but also structural fat creation. What are you making your tissues out of?
Your brain is primarily made of... The solid weight of the human brain primarily made from fats. What are you making your stuff out of? And we know again, this ultra-processed version of so-called vegetable oils significantly increase our risk of inflammation of heart disease. In a study that was published in the journal, Inhalation Toxicology found that even inhaling the smell of Canola Oil, even inhaling the smell of "Vegetable Oil" while cooking can damage your DNA.
Alright, what does that do? Increasing the risk of cancer. So, what kind of oils should we swap out? We already talked about one primary oil, which is Olive Oil. And also, it's proven to reduce inflammation in the brain. Scientists at Auburn University published groundbreaking new research asserting that Oleocanthal Rich Extra Virgin Olive Oil is able to restore the function of the blood brain barrier and help to reduce inflammation in the brain. Now, what if it was our genes that are really the primary cause of obesity like Dr. Fatima Stanford falsely stated in that 60 Minutes segment?
Pretty new study cited in the Journal of Translational Medicine found that Olive Oil can actually help to down-regulate the expression of the FTO gene associated with excess body fat and obesity. Scientists found that a four-week diet intervention that included high amounts of Olive Oil appears to have epigenetic influences that result in improved body composition. Now, the oils are so important because they are so rapidly assimilated by our tissues and utilized for different processes. Even we have trillions of cells in the human body. Fats are needed to maintain our cell membranes.
And in some ways, they're kind of the brain of the cell. When I was in college, it was the nucleus but with the nucleation, we could take the nucleus out and the cell still survives, could do a lot of the same functions. The membrane of the cell is really keeping things together. It's involved, it's kind of like a cellular nervous system in interacting with the environment, having signals on the surface of it, being able to communicate with other cells. The list goes on and on. The cell membrane is very important and so fats are very important. Another fat to target is MCTs, Medium-Chain Triglycerides. Data cited in the International Journal of Obesity and Related Metabolic Disorders found that MCTs have been found to boost the oxidation of stored body fat while increasing satiety at the same time. That's what GLP-1 does. Another randomized, double-blind study published in the same journal placed participants in a reduced-calorie diet that included either supplemental MCTs or supplemental LCTs, or long-chain triglycerides. After the data was compiled. It was revealed that the group who included MCTs lost more weight, eliminated more body fat and experienced higher levels of satiety.
And what could be overlooked in this study is that participants utilizing MCTs were found to retain more of their muscle mass during the weight loss process. Don't go for the random knockoff if you're going for MCT oils. Get it from the best source. Onnit has the best MCT oils out there, period. I have it pretty much every day. You can blend it into your coffees, smoothies, tea things like that, but it's because of the sourcing. Alright, so this is coconut derived. It's taking the concerns out of sourcing like where is it coming from? Making sure that it's done with efficacy and high levels of ethics. And you also get 10% off their MCT Oil and everything else they carry.
I'm a huge fan of their fitness equipment as well. I have a gang of their fitness equipment. You get 10% off everything. Go to onnit.com/model. That's O-N-N-I-T.com/model. The MCT Oil is one of my absolute favorite things. They have the original MCT Oil, then they have emulsified MCT Oils that are kind of like a swap for a coffee creamer or something like that. So again, onnit.com/model. And finally, number three, use your muscles. We don't just store excess energy in our fat cells. We also store it in the form of glycogen in our liver and in our muscles specifically. Upwards of 80% of glucose disposal is going into our skeletal muscle as a healthy individual. That's what's happening.
Now, what happens when we don't have adequate amounts of muscles and or don't use our muscles sufficiently? Where does all of that glucose now go? That's right. This is when we start to develop insulin resistance. This is when we start to preferentially have to shuttle things into our body fat cells. This is when we have this dysfunction at its core. One of the foundational pieces is making sure that we have adequate amounts of muscle because this is where upwards of 80% of glucose disposal is happening. Worse yet, if you proactively eliminate your own muscles, haphazardly not realizing what you're doing, what do you think's going to happen?
Well, you might be like, "Well, I wouldn't choose to lose my muscle tissue." Well, a study published in the Annals of Internal Medicine, this was a randomized crossover study. So, participants went through both trials, both conditions within the study. Over the course of 14 days in one setting, they have a moderate calorie restriction and they're allowed to get eight and a half hours of sleep. The other setting, moderate calorie restriction, same diet but now they sleep-deprived them. They take away three hours and they're only allowed to get five and a half hours of sleep.
The researchers found that sleep deprivation altered the way that their body burned energy. Being sleep-deprived decreased their actual loss of weight from fat by 55%. Alright, so it decreased the weight that they were losing from fat, because they're still losing weight by 55%. Now, here's what's scary. Being sleep-deprived increased their loss of fat-free body mass primarily from their muscle by 60%. Being sleep-deprived was effectively burning off their muscle tissue. And again, one of the things that helps us to defend our bodies against the loss of muscle is to, number one, use our muscles, proactively focus on building healthy muscle and not engaging in activities like repeatedly sleep-depriving ourselves that's going to just burn away our muscle tissue, which is so valuable.
So again, these are three simple principles that are foundational to addressing our obesity epidemic. If we're not addressing these very powerful epigenetic influences, we're talking about things that our genes expect from us for healthy expression, like movement, for example. If we're not doing these things and then coming in with a blunt instrument in the form of one of these newly invented obesity medications, we're going to have to see how this plays out. But we've already really broken down and articulated that this doesn't look very good, right? On the surface, short-term, yeah, people can lose weight, but long-term, we've got to keep our eye on this because our bodies tend to keep score.
So hopefully this has added some empowerment and insight to your day, to your mission, to your journey. Please share this with the people you care about. And listen, we've got some incredible masterclasses and world-class guests coming your way very, very soon. So, make sure to stay tuned. Take care, have an amazing day and I'll talk with you soon.
And for more after the show, make sure to head over to themodelhealthshow.com. That's where you can find all of the show notes, you can find transcriptions, videos for each episode and if you've got a comment, you can leave me a comment there as well. And please make sure to head over to iTunes and leave us a rating to let everybody know that the show is awesome, and I appreciate that so much. And take care. I promise to keep giving you more powerful, empowering, great content to help you transform your life. Thanks for tuning in.
Maximize Your Energy
Get the Free Checklist: “5 Keys That Could Radically Improve Your Energy Levels and Quality of Life”
HEALTHY MEALS EVERYONE WILL LOVE
The Greatest Gift You Can Give Your Family is Health
When you gather your family around the table to share nutritious food, you’re not only spending quality time with them - you’re setting them up for success in all areas of their lives.
The Eat Smarter Family Cookbook is filled with 100 delicious recipes, plus the latest science to support the mental, physical and social health of your loved ones.













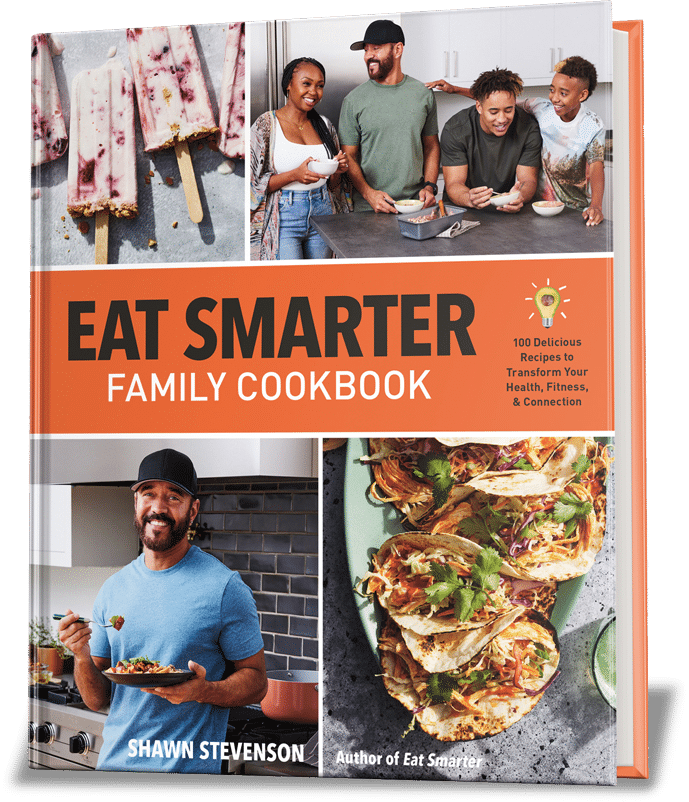
Share Your Voice
0 comments. Be the first to leave a comment.