Subscribe to The Model Health Show:
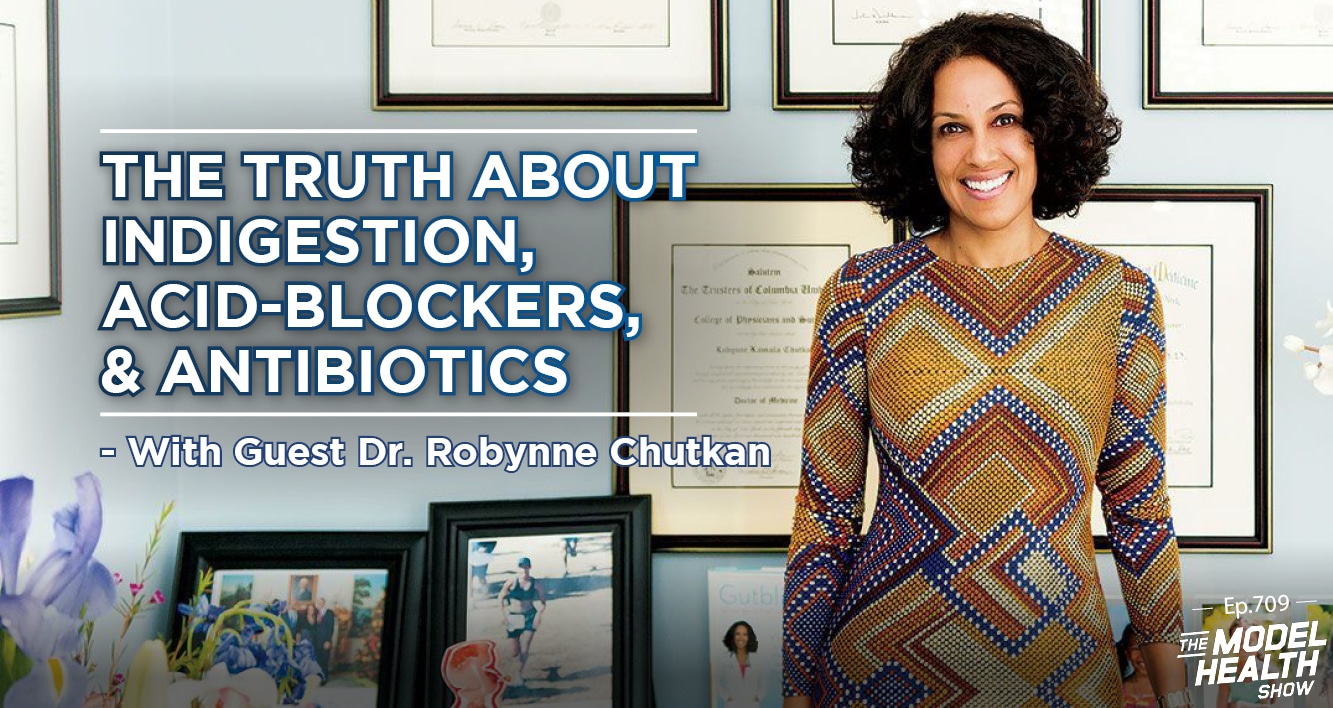
TMHS 709: The Truth About Indigestion, Acid-Blockers, & Antibiotics – With Dr. Robynne Chutkan
There is a myriad of ways in which our Western diet and lifestyle are depleting our health, including their impact on gut health. Both your gut microbiome and the integrity of your gut lining are key components of your overall health, affecting your immune function, inflammation levels, and risk for chronic diseases. On today’s show, you’re going to hear a wealth of insights on how (& why) to improve your gut health.
On this compilation episode of The Model Health Show, you’re going to hear three of the most profound messages from my past interviews with integrative gastroenterologist, Dr. Robynne Chutkan. She is the author of multiple digestive wellness books, including Gutbliss, The Microbiome Solution, & The Anti-Viral Gut. Dr. Chutkan is one of the most influential figures in the gut health space for her practical and effective approach to combating common digestive symptoms naturally, replenishing the microbiome, and building resiliency.
You’re going to hear the cutting-edge science on optimizing gut bacteria, the problem with some of the most commonly prescribed drugs in the US, how to quickly improve the health of your gut, and so much more! I hope you enjoy this knowledge and practical tips from the one and only, Dr. Robynne Chutkan!
In this episode you’ll discover:
- The adverse effects of taking proton-pump inhibitors for acid reflux.
- Why stomach acid is one of your body’s most powerful tools.
- Six common foods that can cause gas and bloating.
- The role alcohol can play in digestive distress.
- An interesting difference between male and female digestive anatomy.
- How the menstrual cycle can affect digestion.
- Why rates of ulcerative colitis and Crohn’s disease are increasing.
- The role diet plays in autoimmune digestive diseases.
- A shocking link between antibiotic overuse and cognitive decline.
- Questions to ask your doctor before taking antibiotics.
- What polypharmacy is.
- The intimate connection between the immune system and the gut.
- What terrain theory is.
- Why your stool is an important indicator of your health.
- The connection between poor COVID-19 outcomes and obesity.
- Why we need to approach obesity as a societal issue.
- How your mucus acts as one of your body’s key defense systems.
- The best ways to promote healthy mucus production.
- What percentage of the human genome is viral.
- The power of eating fermented foods.
- How nature can support your microbiome.
- Things to consider about your medications and the role of your physician.
Items mentioned in this episode include:
- PiqueLife.com/model — Get 15% off any subscription + free shipping!
- EatSmarterCookbook.com — Preorder the cookbook today & claim your bonuses!
- Hidden Causes of Digestive Issues with Dr. Robynne Chutkan – Episode 251
- How Antibiotics Can Damage Your Brain with Dr. Robynne Chutkan – Episode 582
- The Anti-Viral Gut with Dr. Robynne Chutkan – Episode 626
- Gutbliss by Dr. Robynne Chutkan
- The Microbiome Solution by Dr. Robynne Chutkan
- The Bloat Cure by Dr. Robynne Chutkan
- The Anti-Viral Gut by Dr. Robynne Chutkan
- Dr. Robynne Chutkan on Instagram
Thank you so much for checking out this episode of The Model Health Show. If you haven’t done so already, please take a minute and leave a quick rating and review of the show on Apple Podcast by clicking on the link below. It will help us to keep delivering life-changing information for you every week!
Transcript:
SHAWN STEVENSON: Welcome to the Model Health Show. This is fitness and nutrition expert, Shawn Stevenson and I'm so grateful for you tuning into me today, the person who's often considered to be the father of modern medicine is Hippocrates. Now, I don't know if he'll be proud of being the father of modern medicine, but if you look into some of his teachings and some of his greatest messages, for instance, Hippocrates stated that, all disease begins in the gut. All disease begins in the gut. Not in the foot. Not in the pinkie toe. Not in the neck. In the gut. Now, if this holds true, could this be at the core of our epidemics of chronic diseases that we're seeing today, according to the CDC, and this was recently published this year, according to the CDC, six out of 10, 60% of United States citizens have at least one chronic disease, at least one, 40% of our citizens now have two or more chronic diseases.
This is incredibly abnormal. Now, if we were circling back to the father of modern medicine, the baby daddy of modern medicine, Hippocrates, saying that all diseases begin with the gut, if this holds true, could this also be the place to point our attention to help to heal our epidemics of chronic illness and the information that you're going to learn today, and our expert that I have for you is going to shine an incredibly bright light on the situation and provide a wealth of insights, tools and strategies to, yes, improve the health of your digestion, your digestive track, your microbiome, but also help to insulate your body, your tissues, your cells against chronic debilitating diseases and even infectious diseases, and she's got the signs to back it up.
Now, if we're talking specifically about gastrointestinal diseases, listen to this stat, a study that was published in the Journal of Gastroenterology determined that approximately 70 million Americans are now suffering with digestive issues. In 2009, back in the day... This is quite a while ago. We're getting close to about 15 years ago as of this recording, in 2009, there were over 245,000 deaths from digestive diseases. Now, this was data published by the National Institute of Diabetes and Digestive and Kidney Diseases, coupled with the NIH, of course. Now, again, that's getting close to 250,000, a quarter of a million people dying from digestive diseases specifically, are we just going to sit back and allow this to continue to happen, these issues continue to grow. And this was in 2009. Do you think things have gotten better or worse since that point, and you already know the answer to this. And this is why this information is so important, and I'm so excited to share this with you today. Now, before we get to our special guest, I want you to understand something very clearly, when it comes to nutrition, one of the most profound things that rapidly changes your state of metabolic health, the state of your microbiome is things that are in liquid form.
Now, it just make sense because it hits your systems so much faster, it is processed via your stomach, via your small intestine, large intestine, it's assimilated a lot faster because your body doesn't have to do a lot to try to break this material down if it's in food form, and so the liquids that you're consuming really, really matter a lot, if you're consuming sodas, for example, oh my goodness, you are very likely to be experiencing chronic consistent blood sugar derangement and all manner of trickle-down effects from that, be it excess body fat, be it hypertension, be it pre-diabetes or diabetes, the list goes on and on and on. Liquid sugar is different, literally. Now, the same thing holds true for healthier things, for health affirming things versus health detracting things in liquid form. Now, is there a beverage that can actually help to recalibrate and support and improve the health of our gut and our microbiome? Well, I'm here to tell you that there absolutely is. A recent study published in the peer-reviewed journal, Nature Communications, uncovered that a unique compound called Theabrownin found in a traditionally fermented tea called pu-er, has remarkable effects on our microbiome.
The researchers found that Theabrownin positively alters our gut microbiota, that leads to a reduction in hepatic fat, so this is liver fat and reduces lipogenesis, which is the creation of fat. Lipo, meaning fat, and genesis, meaning creation. Now, another study published in the Journal of Agriculture and Food Chemistry found that pu-er may be able to even reverse gut dysbiosis by dramatically reducing ratios of potentially harmful bacteria and increasing ratios of beneficial bacteria. Now, when you hear about a tea like this, as with anything, you should be thinking about sourcing, about quality, because the tea industry is one of the most under-regulated industries, and there's a lot of problems, even with teas that may be labeled as organic, they can have micro-plastics, they can have potential residues, they can have heavy metals. There is one company that's doing a triple toxin screen for common toxicants, and they use a patented cold extraction technology for their pu-er tea.
And this helps to increase the vital nutrients available that get all those benefits for the microbiome that we've been talking about, it's wild harvested as well, so again, beyond organic, that's what we really want. Head over to Pique Life and get the very best pu-er tea on planet Earth, go to piquelife.com/model, and get up to 15% off, free shipping and other bonuses like free tea samples when you try their new pu-er tea bundles. Go to piquelife.com/model, that's P-I-Q-U-E-L-I-F-E.com/model. Again, get up to 15% off, free shipping and other bonuses with their new pu-er tea bundles. Alright, I love those guys. They have the highest standards and over 20 award-winning tea flavors to check out, that's piquelife.com/model. Now, let's get to the Apple Podcast review of the week.
ITUNES REVIEW: Another five-star review titled, “wonderful show” by Horsey Girl, 22-22. “I love this show, Shawn is so positive, honest, and dedicated to bringing great information on life and healing to everyone. His delivery is easy to listen to, and his gifts are amazing. Thanks, Shawn, for bringing us so many great episodes of The Model Health Show.”
SHAWN STEVENSON: Thank you so very much. It's truly my honor, thank you for leaving that review over on Apple Podcast, and now let's get into this powerful compilation of conversations with one of my truly dearest friends in the health space, Dr. Robynne Chutkan. Now, Dr. Chutkan is a board-certified gastroenterologist and author of several best-selling books. She received her bachelor's degree from Yale University and her medical degree from Columbia College of Physicians and Surgeons, where she also did her internship in residency and served as Chief Resident. No big deal. Just a high performer, alright, no big deal. Just somebody who is a high-achieving individual, now, she completed her fellowship in Gastroenterology at Mount Sinai Hospital in New York, and she's been on the faculty at Georgetown University Hospital since 1997, but there was a profound shift in her practice and in her focus, and in 2004 she founded the digestive Center for wellness and integrative gastroenterology practice, dedicated to uncovering the root cause of gastrointestinal disorders. And Dr. Chutkan has also authored dozens of peer-reviewed studies and academic journals, she's been featured everywhere, major media, from the Today Show to CBS this morning, The Doctors, PBS Specials, the list goes on and on and on.
But Dr. Chutkan is, again, a great friend and somebody that we are constantly sending each other things back and forth, different new research, having conversations offline about these things, and she's a real one, I'm telling you, because you sometimes don't really know for certain if somebody's congruent with what they're talking about, and are they really standing up for our families, are they're really standing up for our citizens? And Dr. Chutkan is definitely one of those people, and so I wanted to put together some of the most valuable insights from our conversations over the years, and this is a game changer when it comes to mastering the health of your microbiome and your gut health. There is nobody better on planet earth than Dr. Robynne Chutkan. Now, to kick things off, you're going to hear from Dr. Chutkan on the surprising truth about the multi-billion dollar class of drugs called Proton Pump Inhibitors or PPIs used to treat things like heartburn and acid reflux, you're also going to learn about some of the surprising causes of bloating, you're going to hear the anatomical differences between men and women that influence digestive issues, this blew my mind, and a lot more, check out this first segment with the one and only Dr. Robynne Chutkan.
DR. ROBYNNE CHUTKAN: And I'll tell you, Shawn, I distinctly remember the first time I realized that these drugs that we tend to prescribe like candy were really a problem, it was about 15 years ago at a Food as Medicine Conference with my friend, Gerard Mullin, who's an integrative gastroenterologist at Hopkins, a great guy. He's got some great books out. He started talking about the effect of acid blockers on the microbiome, and if you think about it a dozen years ago, 15 years ago, nobody really knew much about the microbiome work, or rather we knew about it, but we didn't know how important it was, and I remember listening to Gerard's lecture and just being riveted and realizing we are actually creating disease with a lot of these drugs. So let me walk you through what happens when you're on...
SHAWN STEVENSON: Please.
DR. ROBYNNE CHUTKAN: An acid blocker, a potent to acid blocker or what we call Proton Pump Inhibitors, the little purple pill and others, and keep in mind that these drugs are amongst the most commonly prescribed drugs in the world, because when people have acid reflux and they take these drugs, these drugs really very effectively and efficiently block stomach acid, and what that means is you don't get that natural feedback that's so important from your body to tell you that something's wrong when you're having a porterhouse steak and mashed potatoes with cheese and a couple of scotches at 10 o'clock at night and you don't feel well, that's a really important sign, that's important feedback that your body is giving you to protect you from doing it over and over again.
And so, when you remove that negative feedback, you can really induce some damage, so these drugs block stomach acid virtually 100%, and stomach acid is important for some really big reasons, number one, they provide the ideal pH to digest food. So when you don't have any stomach acid, you get maldigestion where you're really not absorbing and assimilating the nutrients properly, and we know that because we know people who are these drugs for years and years, or even sometimes for months can end up with iron deficiency, they can end up malabsorbing fat-soluble vitamins like A, D, E and K, and this can actually lead to osteoporosis and osteopenia and so on, so this could lead to bone issues, because not absorbing vitamin D and calcium and other things properly. So maldigestion is a big one. The other thing is that having an acidic pH provides ideal pH for the digestive enzymes to work properly, so now the enzymes are trying to function in a different pH and that's not quite ideal. But for my purposes, one of the biggest issues with them is that they cause and overgrowth of gut bacteria because they transform the stomach from a pretty hostile acidic environment where excess bacteria don't like to hang out, to a very friendly alkali inviting environment.
Now, you have overgrowth of gut bacteria in the wrong part of the GI tract, gut bacteria really, as we go from North to South, from the mouth all the way down, the amount of gut bacteria increases, so they should really be concentrated in the colon, but instead, you have increasing levels of gut bacteria in the stomach and the small intestine, and a form of dysbiosis called SIBO, small intestinal bacterial overgrowth, it's really an imbalance issue, so these drugs can really create this problem or they can compound the problem in somebody who has other risk factors like taking antibiotics, being a picky eater and so on, and I'm so glad, Shawn, when you talked about your story, you mentioned this sort of background of dysbiosis, because I see that so commonly, people might be struggling with thyroid issues or lactose intolerance or celiac disease, or Crohn's, but there is a background of alterations in the gut bacteria and microbial sort of disarray, dysbiosis, essentially. And so even if they remove the lactose or get rid of the gluten, sometimes they're still not better because they haven't dealt with the imbalance, so it's such an important point.
SHAWN STEVENSON: So, let's shift gears and let's talk about something that's a little bit more probably off the radar for people when it comes to bloating, let's talk a little bit about how alcohol plays into this equation.
DR. ROBYNNE CHUTKAN: This is a sad one. In the first book, Gutbliss, I talked about sad gas as six of the things that can bloat you, and the sad part is soy, artificial sweeteners and dairy, and the gas part was gluten, alcohol and sugar or as some of my friends like to say, well, what else is there to eat besides gluten, alcohol and sugar.
SHAWN STEVENSON: Exactly.
DR. ROBYNNE CHUTKAN: But alcohol can be really problematic on a number of levels, it typically causes you to retain water, so in addition to causing bloating in the belly, it can make you puffy all over. And so that's one way that it can cause bloating, it also damages the liver in excessive amounts, and most people would be surprised to realize that excessive amounts for women equal one or more drink per day, so seven or more drinks in a week, and for men, it's around 10 or 12. So alcohol really puts a... Sort of taxes the liver, and when you think about all the other drugs that people are often taking that are metabolized through the liver, whether that's a prescription drug or a supplement that can really put to a toxic load on the liver, and that can be a mechanism by which people get bloating also, alcohol can be very hard on the lining of the stomach, and it can cause a condition called gastritis, which means inflammation of the lining of the stomach, you can get swelling of the tissues and bloating on that basis.
So, from the more mundane, you had a few too many and you're puffy and bloated, to damaging your liver to, causing inflammation of the stomach, lots of ways, and of course, more severe liver damage can lead to cirrhosis of the liver where you have a lot of excess fluid in the abdomen called ascites and you're super bloated.
SHAWN STEVENSON: Wow. This one is, this is a tough pill to swallow, and it's just, again, everybody, this doesn't mean that you can't enjoy some alcohol, but it's to be aware that this might be causing an underlying problem, and maybe you've tried a lot of other things, but now maybe we need to look at the... We'll just say the party time with the one... Because apparently... So, this is a thing that happens. We go out, we have some dinner, we have a couple of glasses of wine, then you come back home and you have a couple of glasses of wine and the wine just continues, it travels from the restaurant to the home, you just have to be aware of these kind of things, and again, it's all good from time to time, but if you're having strange issues with gastrointestinal problems, bloating, maybe even skin problems, we might want to look at what's going on with the alcohol, maybe pull it out for a little bit of time and see if the things start to subside.
DR. ROBYNNE CHUTKAN: Shawn, I was going to say also one of the big issues with alcohol is before there were antibiotics, what was our main way of preventing infection and cleaning wounds, and so I'm cleaning up the operating room, it was alcohol. So, alcohol has antiseptic properties and it is bactericidal, it kills bacteria. When you go to get your blood drawn, they put that little swab on your arm to clean it, and that's alcohol, so the same way alcohol exteriorly can get rid of germs, alcohol is getting rid of a lot of essential bacteria in the gut when you're drinking it.
SHAWN STEVENSON: Wow. And shout out to anybody who might be drinking and listening to the Model Health Show, again, no judgment, no love lost. Again, and there's some benefits, things like wine, there's studies about this, but again, you have to keep everything in perspective, pay attention to your body and keep it moving. Alright, so let's... And on that note of keeping it moving, you mentioned dairy earlier, so let's talk about specifically lactose intolerance, bloating, I think for a lot of people, they can see that being connected, but let's talk about that.
DR. ROBYNNE CHUTKAN: Dairy is really for baby cows when you think about it, right? Dairy is this ideal food that the mother cow produces to help nurse her baby cow to become a thousand pound big, huge grown up cow, and lactose is a milk sugar, it's what it is, and it's why kids tend to really like it because it's broken down into the bloodstream to something that is essentially a simple sugar, and it can create that effect that we all know that we get from sugar, sort of a sugar high when the dopamine receptors get triggered. So, the first thing to keep in mind is if we think about...
How we're designed and how the universe is designed. Dairy is designed for baby cows, not for adult humans. And as a result of that, many, if not most adult humans, the number ranges from 50 to 75% depending on which study read. But most of us lose our ability to digest lactose. We become lactose intolerant, the enzyme lactase that's located in the small intestine along the brush border, and it's sort of precariously located there. Over time, you lose it. Now some things can result in you losing it faster, like a viral infection can wipe it out, certain types of things. Antibiotics can wipe it out. And there's so many people who know they're lactose intolerant, my 12-year-old is guilty of this. She knows she's lactose intolerant, but she's like, "Ah, I still want some ice cream." And she would love me telling you this.
So, she has the worst gas after she eats dairy. And I'm like, Sydnee, something died up in there, [laughter] It is not. Trust me, I know about gas. It's not supposed to smell like that, but she really loves it, and she likes to eat it. And she's a vegetarian, so she... Her options are a little bit more limited. So, I give her a little bit of leeway, but most people have some degree of lactose intolerance like that. And they might be able to tolerate a little bit of yogurt or a little bit of hard cheese. But, you know, they have a big bowl of ice cream or enough pizza, they start to feel sick. And again, I love your message, and it doesn't have to be all or nothing. But you have to really listen to the feedback your body's giving you. And you have to think about your terrain. So, if your terrain is really messed up, alcohol and dairy and sugar and some of these things could be problematic. So, taking a break and taking it out, maybe reintroducing it in a limited quantity later on, can be a really good way to go to figure out if it's part of the problem.
SHAWN STEVENSON: Perfect. Perfect. And so again, everybody, if you've been experiencing some bloating issues, if there's something that even happens occasionally, that's what today's episode is really all about. Looking at some of the possible underlying things that can be causing this issue. And it's not healthy, you know, in the bloating it's a symbol or a feedback from your body that's something is awry and we need to pay attention to that. So, let's move on. And I thought this was so fascinating in the book, the anatomical differences can be part of the reason why bloating occurs more so for women. So, let's talk about that.
DR. ROBYNNE CHUTKAN: The voluptuous Venus colon. So, for years, I would hear my male colleagues tell women that they had a tortuous colon or a redundant colon. And who wants to be told you have a tortuous or redundant anything? And I came across this information years ago when I was writing a paper for a book. I was writing a chapter on colonoscopy in women. It was a book that was devoted to GI issues in women. And they asked me to do the chapter on colonoscopy. And I realized that women had lower completion rates for colonoscopy. What that means is that there was a higher percentage of times when the gastroenterologist could not get to the end of the colon in woman. And that was true for a woman who had had surgery like a hysterectomy, and so had scar tissue that might've been blocking things or a woman who hadn't had surgery.
And there were a lot of hypotheses floating around about why that was the case. And one of 'em was, well, women just have a lower threshold for discomfort. And having been through 18 hours of labor, hmm. [laughter] I said, I wasn't buying that one. I said, I don't think, I mean people... Pain thresholds vary from person to person, but a generalization like that, that women have a lower threshold.
SHAWN STEVENSON: Yeah, it's crazy.
DR. ROBYNNE CHUTKAN: Just didn't seem to make sense to me. So yeah, I started doing some research and I found three really interesting facts that were not known to me as a female gastroenterologist, not known to my other GI colleagues. I thought, really not known to the general public. And the first is that women have a longer colon, an average of about 10 centimeters longer. Now 10 centimeters might not seem like a lot, but it leads to a lot of extra twists and turns, curviness, redundancy if you want to use that term. But it leads to a lot of extra twists and turns. And so, it makes colonoscopy in women more challenging. I mean, the truth is, it takes me typically about twice as long to do a colonoscopy in a woman as it does in a man because of the configuration of the colon. And why do women have longer colons? We're not sure, but we think part of it might be so that they can absorb more water during childbearing to keep the amniotic fluid replenished. So, the longer the colon is one important factor. The second thing is that women have a wider, deeper pelvis. And again, to allow for childbearing and without wider, deeper pelvis, most of the colon lies deep in the pelvis in women. And what else is in the pelvis? We've got a lot of plumbing. We've got a bladder, a uterus, fallopian tubes, ovaries. And so, the colon has to wrap around all these organs, and it's really crowded down there.
And that's why in women, the first part of the colonoscopy, the sigmoid colon, which is low down in the pelvis, takes a really long time. Men, you guys just have a bladder and a itty bitty prostate. And that's it. So, it's a quick just, you know, I compare it to a horseshoe in men versus a six flags rollercoaster in women.
SHAWN STEVENSON: Wow.
DR. ROBYNNE CHUTKAN: And so that's a second reason, is a wider deeper pelvis and the reproductive organs in women, everything competing for space. The third reason is hormonal. And that's because men have higher testosterone levels. Of course, women, we have testosterone too, just not as much. And higher testosterone levels mean a firmer, tighter abdominal wall. And that's true even for the guy with a big beer belly who doesn't work out just hormonally, he gets a tighter spanx than we do as women. And so that tighter abdominal wall means that, again, it's a firmer spanx to hold everything in and prevent things from bloating as opposed to women who tend to have a more worn out spanx, because our abdominal wall is not as well developed. And so, this is just one of those gender issues that comes up.
SHAWN STEVENSON: Wow. This is, and I'm sure a lot of people, and this myself included, I never thought about this. And I would see people coming into my office, in my clinic and I would see, you know, during certain times of their cycle, we might have constipation, we might have diarrhea happening where they're going more at certain times. And now again, this just all makes sense why it would change like that? And so, let's shift gears and talk about that and how menstruation can be a player in bloating as well.
DR. ROBYNNE CHUTKAN: I love that you're this macho athlete and you are talking about this, this is so important. So, guys, listen up because you need to understand what's going on with your partners and mothers and daughters and so on. Yes. So, the cycle changes...
SHAWN STEVENSON: I've got the biggest smile on my face, by the way. I just... Thank you. Thank you. Go ahead. Go ahead.
DR. ROBYNNE CHUTKAN: The cycle does change with the fluctuating levels of estrogen and progesterone. And that does affect the GI tract also. So, it's exactly as you said, and it tends to be, it can be different from woman to woman, but it tends to be consistent within an individual person. So, a woman will say, I always get diarrhea before my period, and somebody else will say, I tend to be more constipated. So, it tends to be consistent. But it can vary whether it's looser or less loose within the cycle. And we definitely see that variation on a monthly basis. And that's because again, these hormones affect the bowel too. And it's all connected. You know, you can't... Somebody asked me the other day what an integrative gastroenterologist was, and I joked, I said, it's a gastroenterologist who doesn't own an endoscopy suite. So, I'm not trying to just scope everybody who walks into my office, but really, in all seriousness, it is the idea that the body's all connected. Like you, I believe that all disease begins in the gut.
Hippocrates said it thousands of years before we did, but if you think of where the GI tract is, it's really in the center of our bodies. And then all the organs come off like spokes, right? So, the heart and the lungs and the kidneys and the extremities and the brain, they're all spokes on this wheel. And the wheel is really the GI tract. And that's why there's such interplay and such interconnectedness. And you really can't separate it out. You know, you can't sort of just look at one system without thinking about the effect on the others. And particularly for, as I like to call it the below the belt organs, like the colon and the uterus and so on, there's a lot of interconnectivity.
SHAWN STEVENSON: This is so fascinating, just so fascinating. And if we can start to pay more attention to this, again, just paying attention to your body, noticing these patterns I think we could do a lot of good for ourselves, but what would somebody do if they were noticing these patterns? You know, a woman for example, with her cycle where she gets constipated during a certain time of the month. Is this just something to just be aware of and let it ride out? Or is there something that she can do to help to kind of smooth out that transition?
DR. ROBYNNE CHUTKAN: There's definitely things that can be done. And one of the things too for women is to look at what form of contraception you're using. Because if you are on a birth control pill or some hormonal method of contraception, that can be exacerbating what's going on in your gut. So that's one of the first things to look at, to say, hmm, this has been worse in the last six years since I've been taking the pill. Maybe that's contributing even though low dose estrogen pills can cause some bumps in the road. But preemptive treatment is a great thing to do. So, if you know you're going to get more constipated before your cycle, then that might be the time to take a fiber supplement. That might be the time to start doing some green smoothies. That might be the time to do some twisting yoga poses. Ramp up your liquid intake, take a magnesium supplement, which is a great gentle way to encourage evacuation if you will. So, there are lots of things that you can do when you know, right, because knowledge is really power and knowledge is what can make us healthy and have us become our own doctor, which for me is really the goal is that people don't have to come see me 'cause they can figure out what's going on. And so again, there are just so many things that you can do along those lines, starting with dietary changes and then some lifestyle things to help the process along.
SHAWN STEVENSON: Have you seen a trend in this particular condition, which is colitis? I know of course colitis is connected to bloating. But what are you seeing, you know, clinically has this kind of, the rates of colitis gone up? 'Cause that's what I've seen and what's going on behind the scenes with this?
DR. ROBYNNE CHUTKAN: Absolutely. The rates are increasing. So, colitis and the sister disease, Crohn's disease were really described in the 1930s at least Crohn's was by Dr. Crohn Oppenheimer and Ginzburg back at Mount Sinai Hospital. And they were considered rare disorders back then. And we have definitely seen, I have a slide that I use in my talks about the hygiene hypothesis and these modern plagues. So, colitis is a form of autoimmune disease, and like any other-itis, it means inflammation of the colon, colitis, inflammation of the colon. And we have seen an incredible increase in colitis and Crohn's and MS and rheumatoid arthritis and lupus and a lot of these autoimmune diseases. And by definition, an autoimmune disease is a condition where your body is essentially reacting to itself. Your immune system is destroying your body's own tissue. So, in the case of rheumatoid arthritis, it's the joints.
In the case of colitis, it's a colon. And we haven't really been able to figure out exactly why this is. One of the reasons is the food, one of the reasons is widespread use of antibiotics. There have been lots of studies showing that antibiotic use in childhood, especially in the first three years of life and around birth, can dramatically increase the risk of autoimmune conditions like colitis. And we're seeing more and more of that. So that's one thing. Again, the food is another thing. A more processed diet that is low in plant fiber, which is somewhat protective for the colon. But even beyond that, it seems like there are additional factors. And I gave you an example of that. We're seeing more colitis, not just here in the US but in the developing world. And we have our training program at Georgetown, we train a lot of international physicians.
And we were training a physician from Saudi Arabia years ago when I first got to Georgetown about 20 years ago. And I would invite him to come to my colitis clinic. I had an inflammatory bowel disease clinic where I stopped Crohn's and ulcerative colitis. And he said, well, you know, you're fun to hang out with, but I'm going back to Saudi Arabia, and we really don't have this there. And fast forward about seven or eight years later, I saw him at a meeting, and he said, we now have a clinic devoted just to this.
SHAWN STEVENSON: Wow.
DR. ROBYNNE CHUTKAN: At the hospital where I am in Saudi Arabia. So, we're seeing really dramatic increases in colitis in the US but also in the developing world, in Southeast Asia, in sub-Saharan Africa and the Caribbean. And it relates to this idea of the hygiene hypothesis, which I think everybody should know about. And the hygiene hypothesis came about in as a result of a study that Dr. Strachan was doing in England in the 1950s. They were seeing skyrocketing rates of autoimmune diseases, of things like hay fever and eczema in post-industrial London. And they couldn't figure out why. So, he did a study looking at 17,000 kids from birth to adulthood. It's about a 25-year study. And he found two really unbelievable and completely unexpected things that formed the basis of the hygiene hypothesis. The first is that kids from large families where there were a lot of siblings running around, making each other sick, they had low rates of these autoimmune diseases. So being exposed to a lot of germs early in life was actually a good thing.
The second was that the richer kids from more affluent households who were bathing more and these days, affluence does not equal better hygiene practices but back then it did in 1950s London. And so, the kids who were richer and were bathing more and cleaner, they had higher rates of these autoimmune diseases. So, it actually was not a good thing to be too clean, hence my admonition for all of us to live dirtier lives. And so, this turned the whole idea of health and the relationship of germs to health on its head, and this idea that it was actually good to be exposed to germs early on, and it was not good to be too clean. So, what we're seeing in the developing world is that as countries become more industrialized and they start doing things like widespread chlorination of the water, more use of antibiotics, more processed and industrially produced food, and less exposure to these germs early on, is that we start seeing increasing rates of autoimmune diseases.
So, you're a hundred percent right. We are seeing increasing rates of colitis and it's more important than ever that we get this information out and that people really, when you are diagnosed or your kid is diagnosed, or your friend is diagnosed, a loved one, that you say to them, why? You ask that question? We're not good in medicine at asking why. We're good at saying what? So, you have colitis, here's a prescription, come for your colonoscopy, we're done. But you need to ask why. And you need to find that answer out. Was it antibiotics you were given? Is it something you're eating? It never occurred to me 20 years ago when I was doing my GI fellowship, that colitis was something that could be treated through diet. I literally would've laughed in your face if you had told me that. And patients who came in talking about that, I would roll my eyes like, here's another crazy person talking about how they cured their colitis.
The only thing we knew about was a pharmaceutical fix. And what is really sad, Shawn, is that 20 years later, it hasn't changed. I was sitting at the hospital the other day and I was doing; I just finished a colonoscopy on one of my favorite patients. She's amazing. And her colon, she has ulcerative colitis. I diagnosed her 10 years ago in 2007, and I just finished her colonoscopy, and it was normal. Normal and beautiful healthy-looking colon. And one of the GI fellows was sitting next to me and I said to him, take a look at her colonoscopy from 2007, pull up the pictures. And he did. And he was like, "wow, fulminant colitis really active." And the first thing he said to me, he said, well, what is she on? And I said, she's on diet. And I explained to him the diet that she followed, and he was like, but what other, I mean, what, you know, what immunomodulatory drugs is she taking?
And he was so dumbfounded. And this is last week Thursday, Shawn, this is not 10 years ago. He was so dumbfound by the idea that she had put her colitis into remission, primarily through diet, that I took him back there to meet her. And she so generously sat with him for 10 or 15 minutes and answered his questions. And he was like, is it hard? And she's like, yeah, it's hard. And she has three kids. And you know, he asked her what was her motivation for doing it? Was it hard to follow? It was like magic to him. And I think it's a reverse, the idea that you can take a drug and it can magically heal your colitis with no other side effects. That's the magical thinking. So, these drugs, again, can be amazing and they can be lifesaving, but they come with side effects of serious infection and cancer and all kinds of problems.
So, there are times to use those drugs. And I certainly have them in my armamentarium, in my practice. I try to very infrequently write prescriptions for them. But the idea that you would choose a drug that could potentially kill you over trying to control this on your own, that's magical thinking. And that's really the information that I want to get out to people, is that you can actually control your health and what's going on in your body through the choices you make, through the thoughts that you think, the foods you eat, the medications you take, through all the choices you make. And it's such an important message.
SHAWN STEVENSON: Alright. I hope that you enjoyed that first segment with Dr. Chutkan and we've got so much more game changing information to come. Now again, one of the things that I really love about her is that she's truly about that life. She's truly about empowering our citizens, our families, and cultivating these things herself. She walks her talk and she's also created an atmosphere within her household for herself, her husband, her daughter, a culture of family health and fitness. And she's been instrumental in my education and also supporting my projects over the years. In my most recent projects, she's the most excited about that I've ever seen. And she's one of the first person to be able to see it. And it is the Eat Smarter Family Cookbook, and it's coming out very, very soon. I want to make sure that you pre-order your copy. We want to make sure that this is the biggest book of the year. This is the only cookbook that's ever been created that is utilizing over 250 scientific references in the construction of the food of the education. Most of it is centered around social constructs and how it affects our food and our health outcomes. How eating together with friends and family affects our food choices, in particular for our children.
I've got the information, I've got the science to back all this stuff up, but it's all under the umbrella of joy and connection and family and deliciousness. Alright? This is transformation that we get to eat. And I'm telling you, oh my goodness, these recipes are going to knock your socks off. I'm a foodie, alright, but we've been over the years just crafting ways to upgrade our favorite meals and to utilize real food, real food ingredients, and simple recipes. I don't want a recipe that's got 27.8 ingredients. Don't do me like that. I don't got time for that. So again, it's really family oriented, even from the recipe perspective and the driving point of all this is joy. The driving point of all of this is delicious food experiences. And also right now, for a limited time, you're going to get access, when you pre-order the Eat Smarter Family Cookbook, you're getting access to the Family Health and Fitness Summit for free. This is a $297 ticketed event and you're getting it for free, again for a limited time when you pre-order the Eat Smarter Family Cookbook. You'll also receive exclusive online access to the October 2023, Family Health and Fitness Summit. Again, this is a free gift, when you pre-order the book. Lemme just tell you about a few of the experts that you're going to get access to and hear about things like how they're able to create and eat healthy meals with their family, even with a ridiculously busy schedule.
Their biggest secrets for creating a culture of health and fitness in their household. How to find the best deals for groceries, manage picky eaters, get kids involved in cooking and more. You're going to be hearing from World Champion Undefeated boxing champion Laila Ali. And by the way, she's about that life when it comes to food. She won the cooking show chopped twice, and I've gotten the opportunity to eat with Laila many times. Oh, my goodness. Oh, such a great cook. You're going to hear from Vani Harri, New York Times bestselling author. You're going to hear from Dr. Will Ovitz. You're going to hear from Gabby Reese. You're going to hear from Sean T. You're going to hear from Dr. Emy Shaw. I'm telling you; this event is going to be a game changer. So again, you get access to the event for free when you pre-order the Eat Smarter Family Cookbook. Not only that, you're also getting instantly entered into the 25K health and fitness giveaway during book launch week for the Eat Smarter Family Cookbook. Here's just some of the prizes that we're going to be giving away. 500 to a $1000 in groceries from Thrive Market. $500 gift packs from Paleovalley, $500 fitness equipment. Gift packs from Onnit. And those are just a few of things that are going to be given away and you get instantly entered. Plus, other goodies as well.
Definitely pre-order your book right now, support this movement, and I promise you this beautiful book that is so rich in life-changing information, and again, delicious food is going to be a favorite in your household. Go to eatsmartercookbook.com right now to pre-order. That's eatsmartercookbook.com to pre-order your copy of the Eat Smarter Family Cookbook today. Now moving on to our next segment with my dear friend, Dr. Robynne Chutkan. In this segment, she's going to be sharing the shocking new data. That details how antibiotics are being over-prescribed, a new study linking antibiotic use to increasing rates of dementia, the surprising connection between digestive drug usage and COVID infections, and so much more. Check out this next segment from Dr. Robynne Chutkan.
DR. ROBYNNE CHUTKAN: Shawn, this study literally stopped me in my tracks. This was a study that came out in March that looked at frequent antibiotic use in women and noted a significant decrease in global cognitive decline. So, they looked at over 14,000 women. These were female nurses over a period of several years, and they found that women who were taking antibiotics frequently, and when they added it all up, it was for about two months or more over a four-year period, had a seven-point drop in cognitive decline globally. Now, what does a seven-point drop mean? It turns out that's equivalent to about three to four years of aging. It's incredible, right? And so many of us are dealing with issues of family histories of dementia, and concern about cognitive loss. And I don't think that the average person, I don't think the average physician, quite frankly, is aware of these kinds of statistics. And so, one of the things that I'm most evangelical about, if you will, is getting people to understand this connection between the medications they take and the effects on their bodies and their brains. Nothing is free, not even a prenatal vitamin is free. Everything has side effects, and we know that antibiotics are amongst the most over-prescribed drugs in the world.
The Center for Disease Control and Prevention estimates that somewhere around 30 to 50% of antibiotic use in the US is unnecessary. So, people always want to know, I gave a talk yesterday at a women's club and everybody wanted to know what probiotic. I said, draw the brakes for a minute. I don't want to talk to you about what probiotic I want to talk to you about all those antibiotics you're taking that you probably don't need. And you know, my patients, it's sort of a joke, but not really where I say to my patients, if death is imminent, you have my blessing. Otherwise, here are some questions I want to ask your doctor, who's doing the prescribing. Starting with, is this antibiotic absolutely necessary? Is there an alternative? What would happen if I didn't take it? Could we wait? Am I even being treated for an infection? Or you're just giving me this antibiotic to prevent a possible infection? You know, all these things. And I think, unfortunately, Shawn, we're at this point in the medical system where we can't just blindly follow advice. We have to ask these probing questions if we really want to, you know, get to the right place. And we have to be really active advocates in our health and not just rely on the fact that, well, the doctor said, so this must be the way to go.
SHAWN STEVENSON: Yeah, yeah. Here in the United States, especially, you're like a unicorn if you haven't had several stints of antibiotic treatment, especially during childhood. It's just one of those things that's automatic and frequent. And as you said, and I want to lean into this a little bit more because so often it's getting prescribed for things that it's not even valid for. And I think that there might be, you know, there is of course a placebo effect, for example, or things just run their course, but to prescribe antibiotics for viral infection, for example, like even when COVID landed on the scene, antibiotics were getting passed out and there's some really sound data on this that this thing was just getting, again, without any context, this is viral. What are we doing, giving antibiotics for this condition?
DR. ROBYNNE CHUTKAN: Yeah, that, I think that's really kind of the salient point of the last two years. Antibiotics have zero effect against viruses, zero, zip, zilch, nada, none. The only situation where an antibiotic can be helpful in the setting of a viral infection is if you have what's called bacterial super infection, meaning you also have a bacterial infection. And who... Get this, Shawn, this is the crazy part. Who is at most risk for bacterial super infection? People who have been taking lots of antibiotics and don't have enough bacterial foot soldiers to fight the virus. So, the irony is that all these antibiotics people are taking and honestly, I see sophisticated, well-educated people, and when I tell 'em, you know that doxycycline your kid is taking for acne or that Cipro you're taking for sinus infection, do you know that that is dramatically increasing your risk of COVID? They look at me in utter surprise. In utter surprise, and I think what it speaks to is really the power that the pharmaceutical industry has in terms of the marketing dollars. I mean, the money that is spent trying to convince people that these drugs are the answer and the only answer. And we've become so disconnected from our own bodies and our own strength, our own ability to fight these things.
And I have to tell you, that's why I am really such a fan of your show because it really, you know, the goal, the mission is always to educate and empower people to say, you know what, you are actually in the driver's seat here. And that's so true when it comes to infection and you let me know when you're ready to drill down to that whole gut immune connection and how it works because I think once people really understand the relationship, it becomes so clear. The path forward becomes so clear.
SHAWN STEVENSON: Yeah, absolutely. And so, we'll put also up these studies as we go stuff, if people are watching the video version as we go through things today, you could check out the studies. But one of them that I talked about, and this was over a year ago was this huge meta-analysis looking at this phenomenon of something called polypharmacy dramatically increasing your risk of severe COVID. So, polypharmacy is being on multiple medications and they identify three specific types of medications that were tending to be the most pervasive and the most damaging. One of those was related to gut, so the gut medications, so things that are acid blockers, for example, and antibiotics. Why on earth would these be increasing your risk for severe COVID? And one of the things they highlighted in the study was that COVID is at least in part, an enteric infection, a gut related infection because we know there's a lot of ACE2 receptors happening. And also, of course, the immune system, in and of itself is hanging out primarily in that gut environment. So super powerful stuff there.
DR. ROBYNNE CHUTKAN: Yeah, you hit the nail on the head three times, bam, bam, bam. The first is pointing out that COVID is in many ways a gut infection. In fact, we have about a hundred times more ACE2 receptors in our intestines than we have in our lungs. So, the portal of entry is often the gut and that's why GI symptoms in some of the studies are present in up to 50% of people. And we know the virus is excreted in the stool, sometimes for much longer than it's detectable in sputum. So that was nail number one. Nail number two was talking about the acid blockers, Proton Pump Inhibitors specifically. And I think I was on here doing a long rant about these drugs in the past. 'Cause this is just one of my favorite things to talk about because you literally cannot leave a gastroenterologist office. Except mine, of course, without a prescription for one of these drugs, I spend my time on prescribing people. But these drugs are most the common amongst the most commonly prescribed drugs in the world. And part of why they're prescribed so commonly is because they work really well, they're really good at what they do, and what they do is they completely shut off that proton pump, that acid pump in the stomach. So now you can eat your cheeseburger at 11 o'clock and you can have your three cocktails, and you can have your four cups of espresso and you're feeling good, right?
You're like, this is fantastic. The problem is those symptoms, that heartburn that you get when you have your late-night cheeseburger and your four cups of espresso and your cocktails, that feedback is really the negative feedback your body's giving you to tell you, uh-huh, this isn't, this is not a good idea. So, when you remove that, you are actually doing damage and that's what Proton Pump Inhibitors do. When they block the acid, you don't have symptoms. But those symptoms are really important 'cause it's your body signaling you, it's like pain when you overdo it at the gym or a hangover when you drink too much. I mean, I'm always saying, man, if we didn't have hangovers, I mean millions of people would be dying from alcohol poisoning. 'Cause people would just keep going. Right? So that hangover is your body's breaks. And so, what happens? Not only do these drugs remove the breaks, they do something far more problematic in the gut, which is they completely shut down acid production. And acid is digestion 101. You cannot properly break down the food and assimilate the nutrients into your body without acid.
The digestive enzymes don't work at an alkaline pH, so that's one problem. Huge problem now with the pandemic and in addition to the study you are talking about, which is a super important study, there was a big meta-analysis that came out summer of 2020, looking at about 54,000 patients and they found people taking Proton Pump Inhibitors once a day, twice as likely to get COVID, people taking them twice a day, three to four times as likely to get COVID for the simple reason that stomach acid denatures viral protein. It basically renders the virus inactive. If you have stomach acid, so you are happily taking your, little purple pill and eating your cheeseburger late at night and having no symptoms and thinking this is great, not realizing that you have just dismantled one of your body's most potent defense mechanisms against viruses. You have just made yourself so vulnerable. And part of the reason that I love putting this together for people and making sure they understand the connection, is that number one, it's empowering, right? Like now you can understand how to protect yourself.
But number two, people don't know because your doctor gives you this drug. Your doctor is not telling you. By the way, stomach acid is one of your most important host defenses in fighting viruses, and you're not going to have any stomach acid. So not only are you not going to be able to properly digest your food, but you are now going to be much more vulnerable to viruses. And I have these discussions with my husband at the dinner table all the time. He's not in medicine. He's an ex federal agent who does cybersecurity. So, he's kind of my litmus test. And I tell him this stuff and I'm like, you know that right? And he's like, Robynne, people don't know that like, I don’t know that, how would I know that? How would you intuitively know that not having stomach acid puts you at risk for COVID. So, for me realizing people don't know this stuff has really been the main motivation to write these books and get the word out there and be on shows like yours, that with the same goal of we've got to let people know what is happening when they take these drugs.
SHAWN STEVENSON: Yeah, that's, it's probably the biggest thing that has not been addressed this entire time, which is susceptibility and what you can do to dramatically reduce your susceptibility. Again, it puts the power into people's hands. That's the whole concept behind empowerment, but...
DR. ROBYNNE CHUTKAN: Power to the people.
SHAWN STEVENSON: Exactly, and what we've been doing is just creating a psychology of victimization for people. Like I've never seen people in such a victim state as we have the past couple of years, and then that starts to bleed into other things. But also, I'm grateful because I can see how quickly we can devolve into that type of thinking and, leaning into this a little bit more with the susceptibility. I love the fact that, and I'm so grateful you were one of the people who really like brought this front of mind for me, which is that that biological feedback that we get, right? And so, when we are invoking these behaviors, and for me the thing that stands out the most was I had this rendezvous, I had this little intimate occasion where I would go and get this 7-Eleven nacho with chili and cheese, right? And so just psychologically, I didn't realize that it's probably not a good idea to be at this convenience store pumping your meat out of a pump. Right? So, you're pushing, Right. Meat's coming out of this pump is like get some kind of...
DR. ROBYNNE CHUTKAN: Oh, the meat comes out of the pump, not the cheese?
SHAWN STEVENSON: The meat.
DR. ROBYNNE CHUTKAN: The meat...
SHAWN STEVENSON: The cheese too. They were right next to each other. Right. And so, you get the nachos, you pump your meat out, you pump your cheese out. And so, but I would love the taste and how the chips get a little bit soggy. And so, I would take this back to my apartment and have this, you know, this love connection. But every time I would be in pain afterwards, like.
DR. ROBYNNE CHUTKAN: You would feel it. Yeah.
SHAWN STEVENSON: Yes. And my body's telling me, don't eat this. Don't eat this. This is not for you. But what I would do is, because one time I called my mom, I was like, mom, like I just had this 7-Eleven nacho. She was like, just drink a white soda. Right? So now...
DR. ROBYNNE CHUTKAN: That's the one time where mom did not know best.
SHAWN STEVENSON: No. Right. She did not know best. And so now after that, I just start getting my nacho with chili cheese and I get a seven up with it. Right? And still, again, I'm trying to find a way to suppress the symptom. My body saying, do not eat this. This is not for you. And so being able to tune in and listen to that feedback, so the suffering that we get. We've been programmed in our culture to look for a drug or some type of treatment for the thing instead of stop doing the behavior.
DR. ROBYNNE CHUTKAN: Yes. And then you get into the whole polypharmacy thing. You're talking about the wackadoodle. 'Cause you whack that feeling from the liquid meat, nachos, soda combination. You whack it with some Nexium and then you have side effects of the Nexium, and you have to whack that with something else. And then you're whacking the side effects and I, when I have patients come into my office, I have 'em bring all the drugs with 'em. I say, I want to actually see what you're taking. Sometimes they're taking three versions of the same drug. They're taking Nexium, AcipHex and Prilosec. I'm like, this is all the same thing. One doctor gave 'em another doctor, so they're taking multiple drugs and then we get into, why are you taking this? Well, I'm taking this, 'cause when I started this, I wasn't sleeping. So, then I... It's crazy. And I'm like, just stop taking the thing. But it's not our culture. It's our culture is a pill for every ill. Hammer, nail number three, by the way, when you talked about, you made those three really excellent points.
The third one was about the immune system and susceptibility. Why are we so susceptible? So, when I ask people, why do you think that some people get exposed to COVID, never actually even get infected. Others are asymptomatic or have mild symptoms, and others tragically end up in the ICU or even dead. Why do you think that is? Is that random? And you know, there's some obvious things, right? Some people have obesity, some people have a lot of heart and lung disease, and all of these things. But even beyond that, there are additional risk factors and sometimes these risk factors are hidden. Sometimes these risk factors are, you don't have any stomach acids. Sometimes these risk factors are you're taking so many antibiotics, you barely have any helpful microbes left to fight the virus, and so you cannot always tell from the outside, But really one of the most compelling pieces of data was a study that came out last year that showed that looking at the composition of the gut microbiome, Shawn, is 92% accurate in predicting outcome from COVID, 92%. That's more accurate than age, comorbidities like obesity, hypertension, heart disease combined. It's more accurate than looking at inflammatory markers like C-reactive protein, looking at the microbiome and specifically looking at levels of two bacterial. The first is a bacteria called Enterococcus faecalis, which is...
I hate to characterize a bacteria as good or bad, but this isn't a particularly great one to have high levels of because high levels are associated with poor outcome. This is a bacteria that can cross that gut lining into the bloodstream, wreak havoc, and it can allow COVID to do that. And the second bacteria is called Faecalibacterium prausnitzii F prausnitzii. It's my favorite bacteria of all time because it protects you against so many things, against heart disease, against stroke, against colon cancer. And it turns out it protects you against COVID. So, people with high levels of F prausnitzii, the good guy, good girl, have much better outcomes with COVID. So again, this is not random, this is not luck. Sometimes it is, but rarely, you know, we can follow those breadcrumbs back. But here's the thing, again, you can't just go borrow some of your friend's F prausnitzii or take the supplement for the short-chain fatty acids, those important metabolites of microbes that the F prausnitzii is producing, that's keeping your immune system nice and Goldilocks, you know, just right. You have to actually eat the food that the F prausnitzii needs to thrive and to grow and to have a healthy population. And so, you know, people spend so much time trying to figure out, how do I hack this? How do I get a supplement or bar or some stool or, you know, just eat the food. Just eat a little more fiber. It will make a tremendous difference.
SHAWN STEVENSON: All right. I hope that you're enjoying this compilation of conversations with Dr. Robynne Chutkan, renowned gastroenterologist, bestselling author. And in this final segment, which I'm not going to say is my favorite, but it's one of my favorite times, sitting down with her and talking about health and wellness and really extracting some of the actionable things that we can do to transform the health of our microbiome and to protect and support our gut health. In this final segment, she's going to be covering the intimate connection between your immune system and your gut microbes. Why obesity can dramatically increase the risk of severe outcomes from infectious diseases and science-backed ways to improve the health of your microbiome. And more, let's dive into this powerful final segment from Dr. Robynne Chutkan.
DR. ROBYNNE CHUTKAN: Shawn, you know, even in medical school, which for me was a long time ago, I don't think I fully appreciated the relationship between the gut and the immune system. So, let's just start with physically, where is the immune system located? 70 to 80% of it is physically located in our GI tract. So it is, you know, you have the gut lining, that thin membrane with little holes in it to allow nutrients in and waste matter out. And on one side of the gut lining, in the gut lumen, you have the trillions of bacteria and on the other side, separated by a membrane that is literally razor thin. You have all the immune cells and there's constant communication between the two. So, when you think about it, our immune system is exposed to trillions, if not more, whatever the higher number is than that of different organisms that are floating through the GI tract.
Because remember, our GI tract is open to the environment, right? We eat all the stuff that comes through our mouth. And so there are all these microbes, potential toxins, food particles floating around in the gut. And the immune system has to decide which of these things are potentially a threat versus which is just harmless stuff that's coming in. And how is it they decipher that? It's the gut microbes that direct them to say, okay, this is something you need to react to, this is something you can relax, or this is actually helping. So, think of the gut microbes as like air traffic control for the immune system. And so that interaction, that hand and glove relationship is critical for how our immune system functions.
SHAWN STEVENSON: Wow. Wow. So, there's this really, it's a very intelligent system based on our choices, based on the health of this system, of how well it's going to be able to do its job. And so, I would imagine that if there's some derangement happening to be able to assess what a threat is and to properly respond, it's going to be hampered.
DR. ROBYNNE CHUTKAN: Absolutely. So, if you can even sort of physically think about what that looks like, right? So, you have this thin membrane, immune cells on one side, microbes on the other. Think about what happens if there's damage to the gut lining, if those little holes become big. And so, things are coming through now, that communication is disrupted, or think about what happens if the gut microbes, you don't have a full complement or there's imbalance. And I'll give you an example of that. There's a bacterial species called bacteroidetes. And bacteroidetes is one of the gut bacteria that's very important in triggering the immune cells to release cytokines and to sort of start this process, this immune cascade that leads to destroying a pathogen, making antibodies, etcetera. And so bacteroidetes, when they sense certain viral threats, they're in the lining of the intestinal wall right there up against the wall next to the immune cells, and they trigger the release of something called interferons.
And interferons are called interferons because they interfere with viruses, etcetera. So, the bacteroidetes triggers the release of these interferons, and then that starts this immune cascade. So, if your population of bacteroidetes is disrupted, if you don't have enough, if you kill them all off with antibiotics, if you haven't been cultivating a healthy gut bacteria, a healthy microbiome through what you eat, that signaling can't happen. And that immune response may not get triggered. So, it is both a sort of physiological process, but it's also an anatomical physical process that's happening right there in your gut.
SHAWN STEVENSON: Wow, that's so powerful. And also, that category or classification of bacteria is also associated with healthy body composition, insulin sensitivity. But it has this huge role also with the immune system that again, you're really bringing to light versus like that class put up against firmicutes, for example.
DR. ROBYNNE CHUTKAN: Yes.
SHAWN STEVENSON: Which again, everything has its role, but firmicutes are more associated with obesity, insulin resistance.
DR. ROBYNNE CHUTKAN: Absolutely.
SHAWN STEVENSON: And also, dysfunction to the immune system.
DR. ROBYNNE CHUTKAN: And an interesting point about, about firmicutes and evolution is that in people of Northern European ancestry who, you know, thousands of years ago had to endure cold winters, that class of bacteria, that family was more involved with being able to store calories as fat to get through a long winter when food wasn't available.
SHAWN STEVENSON: Wow.
DR. ROBYNNE CHUTKAN: We don't have long winters when food isn't available anymore. Right? So, there's this, you know, evolutionary development of the bacteria, but they're now maladapted to the environment that we live in.
SHAWN STEVENSON: That's so fascinating. It's just like nature finds a way, there's a purpose behind all of these things. But as we'll talk about today, our environment, internal and external today is so abnormal so quickly, it's probably a big reason why we're experiencing what we're experiencing. And in the book, you really highlight that COVID-19, even though the way that the information has been is kind of been propagated and we've been inundated with certain beliefs about things, it wasn't necessarily very indiscriminate. You shared that, and this is a direct quote from the book. "It's less about the potency of the pathogen and more about the health of the host." So, let's talk about that.
DR. ROBYNNE CHUTKAN: Yeah, it's, you know, it came to me that there's a lot of fear around COVID-19 around viruses and so on. And don't get me wrong, there's a lot to be fearful of, especially in the beginning when this is unknown. But what I want to remind people is that for every condition, for every disease or illness, for cancer, for heart disease, for bacterial infection, for viral illness, the health of the host matters. And it matters greatly. If you are an 80-year-old who's a smoker, hypertensive, diabetic, sedentary, overweight, and you get a heart attack, you're going to have a very different outcome from somebody who's 25 and healthy and exercises and is in great health. Right? So, for every condition we're talking about the health of the host, what we call our terrain, what does our soil look like?
So, I like the soil/seed comparison when we think about terrain theory, Pasteur's germ theory says that an organism, a germ, a pathogen gets into our body and makes us sick. And that's true, SARS COVID too can get into our body and make us sick. But terrain theory, which was championed by another Frenchman, Antoine Béchamp, terrain theory says that if our soil is healthy, that seed can pass through our system, may make us a little bit sick, but will recover. We're not going to have the same bad outcome. And we have some fascinating data that really validates terrain theory. So, if you look at one of the landmark studies that was done during this pandemic, it was done looking at microbial analysis as a predictor of outcome. And they found that the health, and not just the health, but the particular representation of certain organisms in the microbiome, which was a marker for health, could predict outcome with 92% accuracy, Shawn.
That's way more accurate than looking at comorbidities like heart disease, lung disease, whether you're a smoker, etcetera, combined. Even when you throw in inflammatory markers in the blood, like C-reactive protein, etcetera, you still don't get close to 92%. And what they found was, again, high levels of a bacteria, Faecalibacterium prausnitzii which is a bacteria that is associated with eating a lot of plant fiber was protective. And people who had low levels of Faecalibacterium prausnitzii were more likely to have respiratory failure, be on a ventilator, be in the ICU and even die. And conversely, they found high levels of a bacteria called Enterococcus faecalis, a bacteria that we know can penetrate the gut lining, get into the bloodstream, cause problems, high levels of that one were associated with poor outcomes. So, it's kind of incredible that a little schmear of stool can give you all this information.
But when you think about the fact that your microbiome is a more unique identifier of you than your own DNA, it's not surprising. Right? The microbiome reflects everything about you, where you've lived, what you've eaten, medications you've taken, even your thoughts, because stress is also reflected in the microbiome, can affect the balance of gut bacteria. So, for me as a gastroenterologist, when I was in med school, long time ago, people were like, why do you want to do GI? Like you want to wade around in people stool? Like why don't you do dermatology or opto or something cool. And I'll tell you the gut is having a moment, right? So now I'm like, here's why I wanted to be a gastroenterologist. Like the stool that you think about as gross and waste matter is a treasure trove of information about us, about our risk for illness, about what's going on with our bodies.
SHAWN STEVENSON: Wow. You were super ahead of the curve, you know, [laughter], and this reminds me of this William Churchill quote, there's nothing more powerful than an idea whose time has come. And like you said, the gut is really having a moment right now, and you mentioned 92% accuracy, being able to check what's going on with your microbiome, 92% accuracy in being able to assess your outcomes via a COVID infection. So it's just like this biomarker is so remarkable at telling how your body's going to react to this virus and probably any other thing we're going to be exposed to.
DR. ROBYNNE CHUTKAN: Absolutely. And you know, it's not an accident that some people have high levels of Faecalibacterium prausnitzii and other people have low, that's directly related to diet. So, you can't unfortunately just go borrow some Faecalibacterium prausnitzii from your plant eating friend or from the health food store. You've got to cultivate that. But the beautiful thing about this, Shawn, and the optimistic message, and the reason why I'm so excited to bring this information to people is that you can actually change your microbiome. And you could do it pretty quickly. I mean, you can't change it overnight, but you can make little consistent changes to how you live, how you eat, even how you think, how you sleep, all of these things that can make you healthier and more resilient.
SHAWN STEVENSON: Yeah. It's just start the process. Start today, the best time was probably to start last year, but the second-best time is now. Another quote from your book, you said, "Susceptibility and poor outcomes are almost always predictable and preventable, or at least reducible." Right? So, we... This stuff isn't just random. And seeing, being able to really assess our susceptibility and also our potential resilience under these conditions is really important. And with that said, this leads to another part that you mentioned. Counseling and strategizing about that risk and how to reduce it are much more effective than any drug or medical intervention because medications are critically important for those who need them. But for the majority of us, our body's own ability to resist, heal, and recover from viruses is vastly superior.
DR. ROBYNNE CHUTKAN: And you know, I want to unpack that a little bit because I want to make sure people understand we're not blaming, and I certainly am not blaming anybody for a poor outcome, anybody who gets sick from this viral illness is a tragedy. And certainly, people who have died or who are still suffering with post-viral symptoms, that is a tragedy. But you can acknowledge that. And also, at the same time point out that there are risk factors that we know about. And we don't just know about them because we have sort of pulled it out. We know about them because there is really reliable data behind it. So, if you look for example, at having obesity, we know that is a significant risk factor that is associated with a much higher likelihood of doing poorly. And when you think about it, there's some very clear reasons.
Somebody who has obesity, particularly if they have a lot of central obesity, it's harder for the lungs to expand. So having obesity interferes with mechanical ventilation of the lungs, and this isn't just true for COVID, this is true for pneumonia, for any respiratory illness, there are going to be worse outcomes. And when you can't inflate and deflate your lungs properly, what happens is that bacteria can pool in some of these spaces in the lungs, and you're at high risk for bacterial super infection. So now you have a bacterial pneumonia on top of a viral illness. We know that in people who have obesity, they have factors floating around in the blood, pro-inflammatory factors like clotting factors that can make you more likely to clot and have problems there. We know that adipose tissue itself is immunologically active and is producing sometimes extra cytokines that are leading to an overblown immune response.
You're overshooting the mark and you're ending up with cytokine storm and acute respiratory distress syndrome, etcetera. So we know that there are these medical factors associated with being obese, with having obesity. And it's critically important that we provide people with meaningful tools from a public health, from a policy point of view to help people. And we have to look at this as a collective problem. Somebody being obese is not just their problem. Like, sucks to be you, too bad. You know, if you think about viral shedding, we know that in the setting of obesity, viral shedding can be prolonged by as much as 42% longer. And so, what that means is that somebody who has obesity can be shedding a virus longer. There's more opportunity for transmissibility, and there's more opportunity for viral transformation to potentially a more virulent form of the virus. So, this is a collective problem, right?
We are only as healthy as our least healthy citizen. And so, I think we've seen an incredible spirit of generosity and graciousness with this pandemic with people coming together, helping their neighbors and so on. But I think we really need to take a different approach to obesity in our society. And we need to look at it as it's a problem for our society, not for the individual person only. And what can we do to help our brothers and sisters who are struggling? 'cause It's hard, right? It's very hard, especially if this is something that you've been dealing with from a young age, it's hard to lose weight. And how can we have more resources for people in terms of access to healthy food, access to spaces for leisure, etcetera. And it's particularly important in certain communities. If you look at our African American community, we have extraordinarily high rates. And it's not surprising that those rates are also tied to economic disadvantages, etcetera.
SHAWN STEVENSON: Thank you so much. You just unpacked really why obesity is a risk factor. Because just to be clear, again, this is not about a vanity metric. This is about true human functionality. I love you gave a mechanical example with the lungs, right. But also, you gave that kind of internal, the word inflammation is getting, it's also having a moment right now and talking about how fat cells themselves are kind of sending out a false distress signal when they're under stress because of the contents that they're forced to carry on. And it's putting the body into a pro inflamed state and then a pro-inflammatory virus exposure comes along. What do you think's going to happen?
DR. ROBYNNE CHUTKAN: Boom.
SHAWN STEVENSON: We talked about this. I think I sent you this study early on, but you know, it's one of our conversations over the last couple years. But the CDC did a huge meta-analysis. Over 800 US hospitals, over 540,000 COVID-19 patients, huge set of data. The number one risk factor for death in their assessment is obesity.
DR. ROBYNNE CHUTKAN: Yes.
SHAWN STEVENSON: The number one risk factors, it stood out.
DR. ROBYNNE CHUTKAN: And particularly people under 65, it's way more likely. I mean, the number I believe from one of the large studies was 113% more likely to be hospitalized. 70 something, maybe 76% more likely to be ventilated and a very high number more likely to die. Also. And again, this is something we can do something about. By the way, I love how we exchange these articles and we geek out and I'm like, nobody else is really interested in this, but Shawn and I are like exchanging these texts and like, can you believe that? Look at this. Yeah. Thank you. I appreciate that.
SHAWN STEVENSON: Of course. And we're doing things to, again, get to... I'm so grateful actually for this experience in a way because, and it takes some time to process things of course, but it's giving us an opportunity to really look at our state as a society. I think that especially when we're working towards health and wellness, we can get into our own little bubbles, and we can overlook that so much has been going wrong in the last few decades. The rate of obesity, as we talked about before the show got started in children has tripled since the 1980s. Something is severely wrong here. And we can start to let things linger a bit, when right now something like COVID-19 brings about a sense of urgency to make some changes. Because again, this is the number one risk factor. But we did the thing we tend to do, which is we got to find a drug to try to fix this. And again, just look at the outcomes from that whole thing. And we can try to frame things in a way that, oh, this is successful. But at the end of the day, our constant desire to drug our way into and out of things has led to a situation where, you know...
And this is just, it is what it is. A $4 trillion health care system with pharmaceutical companies making hundreds of billions of dollars, and yet we're the sickest society in human history. Something is not matching up here.
DR. ROBYNNE CHUTKAN: And we are much sicker than countries that spend a lot less money. And here's the thing, I am a conventionally trained doctor, I have an integrative approach. I am all for judicious use of medication. I am delighted personally and professionally, that we have ventilators and monoclonal antibodies and all sorts of things for people who need them. But wouldn't it be so much better if we didn't need that?
SHAWN STEVENSON: Yes, exactly.
DR. ROBYNNE CHUTKAN: If we were healthier and we didn't need that. And the outcome is different, these things can save lives for sure, but again, a healthier host means that you're much less likely to need these things.
SHAWN STEVENSON: Let's talk about, another one of these host defenses. So, we talked about stomach acid, so important. But you talked about something and the way that you articulate in the book was so fascinating. Mucus of all things. Again, we just think it's another one of those dirty words.
DR. ROBYNNE CHUTKAN: Gross, not. And what's funny, when I was going into GI, I had a couple of friends who were going into pulmonology, being lung doctors. And I was like, "Oh my God, snot is so gross." And they were like, "Are you really a gastroenterologist dealing with stool telling us that snot is gross?" So, there was all this sort of battling about which is gross, snot or stool. And now as it turns out, they're both really important. Again, these things, you think snot is something nasty you should blow out or suppress. So, let me tell you about mucus.
First thing that I want people to know is that most of the mucus in our body, the overwhelming majority comes from our GI tract. About one and a half liters a day are made in our gut. So, it doesn't come from our head or lungs, primarily from our gut. And one of the main functions is a lubricant, so the mucus lines the gut, so that as a products of digestion move through, it can have nice smooth transit. It also provides a set of sticky lubricant matrix that lines things and that provides kind of a buffer for things like viruses and toxins to reach that inner lining. They have to wade through this gel.
So, mucus is like this cross between jello and glue. And it is a sticky matrix that traps pollutants and allergens and pathogens, so it can trap pollen and things and smoke, but also viruses. So, the mucus ensnares the virus in the sticky matrix, and then the cilia in the lungs work to move it up and out, and then you either spit it out or you swallow it. And if you swallow it, that's fine, 'cause then your stomach acid is going to do it's thing and denature it. So, not only is mucus physically trapping the virus, but mucus also has proteins in it called mucins. And these mucins have enzymes that can degrade viruses and again, render them inactive.
So, it's a double whammy ride, it physically traps it and then enzymes work on it. It's like a spider web and degrade it. So, if you have good quality mucus, if you stay hydrated, let me take a sip in honor of the mucus. You stay hydrated, you have nice healthy mucus, you don't smoke, you get some fresh air, you eat a healthy diet, all these different things. You have good quality mucus, and your mucus is able to work for you. If you're a smoker, you don't hydrate well, the quality of the air isn't so good where you are, unfortunately, that's not one that people can necessarily do something about. But there are other things that you can, that can really make a difference.
But the biggest issue is again, people sabotaging this by taking a cough suppressant. And so, if you have extra mucus runny nose, etcetera, when you have a cold, it's because your body is fighting something. It is producing that extra mucus to try and trap that. That's why with allergies too with the pollen, your nose will run. Because you're producing more mucus to trap the pollen to get rid of it. To clear it from your body, but what do people do? They don't understand that, and so they take a cough suppressant, they take an antihistamine. They take something to dry out the mucus, and now they are left defenseless in terms of that particular important defense. So, the American Academy of Pediatrics does not recommend, they recommend explicitly against using cough suppressants in kids when they have respiratory illnesses. But that should apply to adults also, and older children.
SHAWN STEVENSON: Most people don't know that.
DR. ROBYNNE CHUTKAN: Is that, then people say, "Well, what am I supposed to do?" Well, I have 10 things for you to do in the book that you can do to help with symptoms. 'Cause the goal isn't just suffer, right. Where I come from in Jamaica, we always say a little sufferation is good. But the goal isn't like just suck it up, there's nothing you can do, there's a lot you can do. But you want to do things without sabotaging this major innate host friends and let the mucus flow.
And what's fascinating, Shawn, and it's fascinating when we think about what's going on with the epidemic, the opioid epidemic. Is that if you look back at the 1800s, like in 1843, Mrs. Winslow Soothing Syrup and Bears, first cough suppressant. Bears product had heroin in it, Mrs. Winslow Soothing Syrup had morphine in it, so these were great at getting kids to stop coughing, but sometimes the kids never woke up. These things from over 100 years ago had narcotics in them, and some of these things continue to have narcotics in them until really the early 70's. So, beyond the issue of, it's going to suppress your mucus and you're not going to be able to trap and expel the virus, you have to think about what else is in this stuff and what is it potentially doing to us.
SHAWN STEVENSON: It's still happening today. People are buying cough syrup for the purpose of finding a high. The psychoactive components to it is so crazy because again, morphine, heroin packaged up in different ways today, the opioid epidemic, which on that list from BMC Medicine of those three most identified prescription medications that are leading to poor outcomes from COVID. Number one was antipsychotics, number two was Proton Pump Inhibitors, number three was opioids. So, we're still doing a lot of the same, it's just packaged up differently, and this is getting back to... I love the fact that you mentioned, even when we have a cough, it is your body's intelligent, it's working towards an adaptation from that exposure.
And this is something that makes us human and makes us more resilient as time has gone on, but we forget that. And you even mention in the book, this is something that we talked about earlier on. The human genome mapping that out, we find that upwards of 10%, 8%-10% of the human genome itself is viral.
DR. ROBYNNE CHUTKAN: Is viral.
SHAWN STEVENSON: As we've evolved and adapted to this exposure and it's going to continue happening, but it's getting ourselves to a place where we understand and identify these symptoms, as these adaptation responses as our bodies are kind of taking on this new sampling, new data and figuring out ways to be more resilient in the environment. But I got to mention this because allergies, you said allergies earlier. And we think, again, we have this innate susceptibility where I look this up, reading your book. This was from the CDC. Alright, the CDC found that food allergies in children... Because again, so much of this is new. It's just happened within the last couple of decades.
Food allergies in children have increased approximately 50% from 1997 to 2011. Something has happened, making us more susceptible to the environment. Whether it's food, whether it's allergens, you're not the same species.
DR. ROBYNNE CHUTKAN: It's a couple of things, and I think when you look at that number, it is both externally, the food is different. There's a lot of edible food like substances being marketed as food, but we are also different. Because our microbiome is different, and if we look at the... And I want to circle back to the point you made about the viral DNA too. But I do want to make this point, if we look at what's going on externally in the environment with climate change, etcetera, and deforestation and over-fishing. And you're literally in the ocean and you don't see any fish, and you look at all the trees being cut down, we are seeing the exact same thing going on in our microbiome.
We have a third less of microbial species than people like the Hadza tribe, our brothers, and sisters in Tanzania or in the Amazon. And of course, in the Amazon and in Tanzania, their habitat is at risk. The environment they live in, that they've relied on for millennia to hunt and fish, etcetera, is under threat. When you look at the aluminium production, bauxite in South America and these red rivers it's created and how it's destroyed the fishing industry, etcetera. So, it's all at risk, and they are facing a whole different set of diseases now as a result of that.
And the same thing, so internally, we are different, we are changing our internal landscape. Not for the better. Not for the better. So, we have to think about that, and as a result, we are seeing allergies, autoimmune diseases, etcetera. But to go back to the great point you made about the virome and 10%, 8%-10% of our DNA being virally derived. When a virus is just genetic material, it's not really alive on its own, but when it infects the cell, it inserts a genetic material into the cell, hijacks the cells machinery, gets the cell to start replicating. It's the original gangster these viruses. Gets the cell to start replicating its viral material.
If it infects a sperm or a gamete, reproductive organ cells, it then gets into our DNA, becomes part of the reproductive process. And some of these viral proteins are responsible for really important functions, like for placental proteins that are involved in reproduction. Proteins that encode memory, there are viral proteins that make us immune to viruses like to other viruses like HIV, to bubonic plague, to all kinds of things. So, if we look at Herpes simplex virus, mice infected with Herpes simplex virus are more resistant to bubonic plague, bacterial infection caused by Yersinia pestis.
And so, are humans. Now, fortunately, bubonic plague is not something knock wood, that we have to worry about at the moment. But it just shows this sort of adaptive evolutionary advantage that exposure to some of these viruses can provide.
SHAWN STEVENSON: Yeah, I love this. So, of course, the most important part of your book, you've got the education component, but also what can we do proactively? What are some of the steps that we can take? Because there are really three major sections in the book, part two focuses on what goes wrong, how all this stuff came to be. And part three of the book, you have the anti-viral gut plan, and you talk about building up your body is one of the highlights of things, securing your defenses. So, let's talk just a little bit about that, give people a brief insight into some of the dos and don'ts for us to support our microbiome, our gut health and just to become more resilient moving forward.
DR. ROBYNNE CHUTKAN: Sure. And I will say, when I wrote my first book, Gutbliss back in 2013. I wasn't even writing a plan, it was really my team at Avery that said, "People want to know what to do, this information is great, but what to do." So, there was a plan. And then second book, The Microbiome Solution is a bigger plan. This book, the plan is, it's part three, but it's almost half the book. This book, I really... I finally have like, I get it, people want to know what to do. And I had so much fun with a plan, Shawn, being really sort of creative about workarounds. So, the food part is maybe the most obvious part. Explaining what are the things, but the nice thing about it, it's less about what you shouldn't be eating, and it's all about what you need to add in.
Add in a tablespoon of a fermented food like sauerkraut, just a tablespoon. It's about 10 grams is going to give you up to 28 different bacterial strains that are all doing really important things. So, it's like a live... It's living food, medicinal food. So, the food one is maybe the most obvious. But if you think about the sleep one, and of course you're the sleep master. If you really want to know how to sleep well, but I did make the connection for people between sleep and the gut. Because as you know Shawn, serotonin, the feel-good hormone is made primarily in the gut, and serotonin is a precursor hormone to melatonin that you need to sleep.
So, there is this incredible connection between what's going on in the gut and sleep and the neurotransmitters who the gut brain access, etcetera. So, I had a lot of fun coming up with, "Okay, here are some things that you can do." And you'll see that melatonin is in there, I talk about it, but it's way down towards the bottom of the list. There is, it's divided into different sections about your environment and habits, etcetera. And then at the bottom, okay, here's some sort of medical supplement type things.
Environmental things, the open-air factor, that's something that people don't talk about. This is something we know from back 100 years ago, with the Spanish flu epidemic. Ironically, with military personnel, the officers were often given a bed inside the hospital to recuperate, and enlisted men were put on little carts outside, like you don't rate, you're just an enlisted guy, you're just going to be in a cart outside. Well, there was a huge difference in the mortality rate, the people recuperating inside had up to a 40% mortality rate in some instances, and outside, 13%. And the reason for that was what is called the open-air factor. OAF, which is defined as a germicidal constituent in open air.
This is different from sunlight and vitamin D. That can be toxic to viruses and some other pathogens, so there are tips in there for... Okay, even if you can't get outside and you do some forest bathing and walk in the woods, you can literally open your car window bringing some outdoor air and that can make a difference. You can poke your head out the window, sit down on the roof, step outside on a balcony, that kind of thing. Exposure to soil microbes, literally putting your hand in some dirt, profound impact on what's going on with your microbiome. So, some of these environmental things are really important also.
So, it is, as you said, it's divided up into sort of building up the body, and also giving people really detailed information, for example. If you're on a Proton Pump Inhibitor, here's a schedule for how to taper off, and here's some tips to help you. Now, of course, people need to do that in conjunction with their health care provider, but really step-by-step detail information. The medication section is the one that I'm really the proudest of, because I tell people, "These are the medications that are problematic." But I don't just say, don't take these medications. I say, here's what you should ask your doctor about what you could take instead including alternate day dosages, different form of this medication that will still be anti-inflammatory but isn't going to be as toxic to your gut microbes, and then here are possible substitution.
So, I give people literally a checklist with detail information that they can take into their doctor's office and say, 'Well, I'm on this, what about that?" And I do that for all the different medications. Because again, and I was wary about it 'cause I'm like, I don't want to be giving really prescriptive advice to people, I'm not their doctor, but I realized people need the information to have that conversation with their doctor. And so, I wanted to make that really easy for people in the book are what are the different things that you could do instead. And it's amazing how much at the time, 'cause I do this with my patients, they may be being prescribed something, maybe their rheumatologist has them on a high dose of ibuprofen or something for joint pain. And I'll say, "This is what I want you to ask them." And they go and ask them. And the doctor is like, "Oh yeah, sure."
And then they come back mad to me saying, "Why didn't they do that in the first place?" And I'm like, "I don't know. But they're doing it now." So, I want people to have that dialogue. It shouldn't be a monologue. If you go to see a doctor and they're just talking at you and it's not a conversation, and you're really not able to exchange ideas and information with them and get their opinion and feedback, you need to find a new doctor.
SHAWN STEVENSON: Thank you so very much for tuning in to this episode, I hope that you got a lot of value out of this. Isn't Dr. Chutkan an amazing? I love her so much. If you enjoyed this, please share this out with your friends and family and share this on social media. Take a screenshot of the episode and tag me, I'm @Shawnmodel, tag Dr. Chutkan in as well, she's @gutbliss on Instagram, probably the best handle. That's top 10 handles on Instagram. And just share the love with her, I'm sure that she would absolutely enjoy that.
Alright, and of course, you can send this directly from the podcast app that you're listening on as well, to somebody that you care about. And listen, we've got so much more in store for you, so make sure to stay tuned. We've got some epic world class guests, powerful master classes. And of course, we've got the Eat Smarter Family cookbook coming very, very soon. Head over and pre-order your copy and get those bonuses right away. It's eatsmartercookbook.com. And again, be ready, we got so much more in store for you, so make sure to stay tuned. Take care, have an amazing day, and I'll talk with you soon.
And for more after the show, make sure to head over to themodelhealthshow.com. That's where you can find all of the show notes, you could find transcriptions, videos for each episode, and if you got a comment, you can leave me a comment there as well. And please make sure to head over to iTunes and leave us a rating to let everybody know that the show is awesome, and I appreciate that so much. And take care, I promise to keep giving you more powerful, empowering, great content to help you transform your life. Thanks for tuning in.
Maximize Your Energy
Get the Free Checklist: “5 Keys That Could Radically Improve Your Energy Levels and Quality of Life”
HEALTHY MEALS EVERYONE WILL LOVE
The Greatest Gift You Can Give Your Family is Health
When you gather your family around the table to share nutritious food, you’re not only spending quality time with them - you’re setting them up for success in all areas of their lives.
The Eat Smarter Family Cookbook is filled with 100 delicious recipes, plus the latest science to support the mental, physical and social health of your loved ones.













Share Your Voice
0 comments. Be the first to leave a comment.