Subscribe to The Model Health Show:
807: Shrink Your Fat Cells & Fix Your Metabolism – With Dr. Benjamin Bikman
Most people understand that metabolism is a key factor in controlling weight and overall health. But the science of how the metabolism actually works can often be confusing or oversimplified. On today’s show, we’ve got one of the world’s leading authorities on metabolism here to break down the inner workings of insulin, blood glucose, and more.
Metabolic scientist and professor Dr. Benjamin Bikman joins us on this episode of The Model Health Show to unpack the critical role that insulin resistance plays in obesity and chronic illness. You’re going to learn the exact mechanics of how insulin resistance occurs in the body, and realistic lifestyle interventions you can implement for better metabolic health.
This interview contains key insights on fat loss strategies, how dietary factors impact metabolic health, and the interesting details of Dr. Bikman’s research studies. Today’s episode is absolutely packed with the latest science on metabolism, so click play and enjoy the show!
In this episode you’ll discover:
- The connection between insulin and type 2 diabetes.
- Which two markers are important for measuring metabolic health.
- How Dr. Bikman’s study helped participants reverse diabetes.
- Why insulin is a unique hormone in terms of how it impacts cells.
- The connection between insulin resistance and infertility.
- What the three primary causes of insulin resistance are.
- How cortisol and adrenaline impact insulin levels.
- The important role that sleep plays in insulin sensitivity.
- Which cause of insulin resistance is the most common.
- The effect each macronutrient has on insulin levels.
- How long insulin circulates in the body after eating.
- The natural rhythm of cortisol levels.
- How exercise impacts blood glucose levels.
- The best exercise for metabolic benefits.
- Why fat cells cannot grow without insulin.
- How cold water immersion impacts the metabolism.
- Four main dietary principles for better health.
Items mentioned in this episode include:
- Onnit.com/model — Save an exclusive 10% on performance supplements & tools!
- Plunge.com/model — Use code MODEL150 to save $150!
- How Not to Get Sick by Dr. Benjamin Bikman & Diana Keuilian — Get your hands on this new book today!
- Why We Get Sick by Dr. Benjamin Bikman — Grab a copy of Dr. Bikman’s first book!
- Sleep Smarter —Upgrade your sleep habits with strategies in my national bestselling book!
- Connect with Dr. Benjamin Bikman Website / Facebook / Instagram
This episode of The Model Health Show is brought to you by Onnit and Plunge.
Visit Onnit.com/model for an exclusive 10% discount on human performance supplements and fitness equipment.
Get your very own cold plunge by visiting plunge.com/model and using my code MODEL150.
Thank you so much for checking out this episode of The Model Health Show. If you haven’t done so already, please take a minute and leave a quick rating and review of the show on Apple Podcast by clicking on the link below. It will help us to keep delivering life-changing information for you every week!
Transcript:
SHAWN STEVENSON: There's a critical metabolic fact about fat loss that many people simply don't know. Your body simply will not release stored body fat if insulin is active. When we hear the word insulin, we usually think about it in terms of metabolic conditions like diabetes, type one diabetes and type two diabetes. But insulin is one of the most important hormones for life as a human being. We need insulin to survive. It is the hormone of storage. But again, when insulin is active, in particular, when it's overactive and when our cells lose sensitivity to insulin, this creates a blockade in our fat cells ability to release their contents.
Again, insulin being the hormone of storage, we cannot release when insulin is doing its thing. So with that being said today, you're going to get a masterclass from one of the world's leading authorities on metabolic health and specifically on the role of insulin. You're going to hear about his study that was published in the Journal of Diabetes Research where he and his team took test subjects with type 2 diabetes and effectively reversed their type 2 diabetes within a 90 day period, complete remission. They no longer had diabetes at the end of the study. You're going to find out how exactly he did that. Again, this is published peer reviewed data. This exists. Type 2 diabetes does not have to be a death sentence, let alone a condition that you have to live with. We, in fact, can completely reverse this condition and getting that knowledge is so important today.
Plus, he's going to cover the three critical components of insulin resistance, and I'm telling you, most people have no idea about these. It's not what you think. And once you understand these and you understand how these three things also lead into every major chronic condition that is killing our citizens today. So all of the top 10 causes of death are rooted in these three things as well. And again, being the foundation for insulin resistance. Plus, and of course, we're going to dive into how do we reverse this condition of insulin resistance? How do we improve our insulin sensitivity? And, one of the craziest, most overlooked parts of this conversation, should we just be looking at blood sugar?
Because that's what we tend to think about, or, can we accurately measure and track insulin itself? And so this interview is filled with game changing insights. And I'm very grateful to dive in this conversation with the amazing Dr. Benjamin Bikman. Benjamin Bikman earned his PhD in bioenergetics and was a postdoctoral fellow with the Duke National University of Singapore in metabolic disorders. Currently, his professional focus as a scientist and professor, and he's at Brigham Young University, is to better understand the role of elevated insulin and nutrient metabolism in regulating obesity, diabetes, and dementia. He's been featured all over major media and his work has been published in several academic journals.
Let's dive into this conversation with Dr. Benjamin Bickman. I'm very excited about this. We've got the foremost expert from my perspective in the world on metabolic health and he's brought something into the Conversation that simply was not getting addressed when talking about insulin resistance. And if you could, can you start off by sharing the study that your team conducted? It was a 90 day study on type 2 diabetics. Effectively putting their condition into complete remission. Can you start off by talking a little bit about that?
DR. BENJAMIN BIKMAN: Yeah, I'd be happy to. Let me, Shawn, just let, just because I'm a professor, I can't help but want to provide just a brief moment of background. Insulin, some people may even be wondering, what's the connection between insulin resistance and type 2 diabetes? Type 2 diabetes is the insulin resistance that's gone so far that now it can't control the blood glucose very well. So just to say that briefly, one more, one more, in one other way. If I have two metrics that I'm looking at clinically, two markers, I have insulin and I have glucose.
Insulin resistance is commonly referred to as pre diabetes because the glucose levels are still normal in insulin resistance in this early stage that we call insulin resistance, but the insulin levels are not. So insulin resistance is high insulin, but the insulin, even though it's not working too well, it's working well enough, albeit at a much higher level to keep blood sugar levels at a normal level. And because we have such a glucose centric view of metabolic health, we miss this problem. And then it's 10 or 20 years later, where the insulin keeps climbing up, and we can, but we eventually get so resistant to its effects, that now the blood sugar levels start to climb, and then the clinician will say, Ah, you've got diabetes.
So just to just set the stage, just imagine how much more powerful our clinical prognostic capabilities would be if we said, okay, glucose is important, but insulin is more important when it comes to being the kind of early canary in the coal mine, the early signal for metabolic health. Now to the study that you'd mentioned, I was particularly thrilled with that study because it was the first time my lab had collaborated with an actual clinical entity. So there was a local clinic whose physician, the physician team, had heard about my research. I'd had dozens of meetings with them, given talks to the clinical team at their actual site. And they were all in, they really had bought into this view. And so working with, we identified 11 patients.
It just coincidentally, they were all female across primarily Caucasian and Hispanic ethnicities. I think we had a couple Asian as well, but just touching on the fact that this is relevant to cross ethnicities and they were given the decision. They had the first choice, which is always the one presented to the type two diabetic at the time of diagnosis, which is you can take a prescription for a medication.
Usually it's an anti diabetic medication like metformin or similar. Nowadays it would be a drug like ozempic probably even maybe the, on the first line here. So that's the typical. conventional clinical process where you are given a prescription for a drug. However, these patients were given a second choice.
You can leave with the prescription for the drug. You'll never get off it for as long as you are relying on the drug to help keep your diabetes managed, it's now a prescription for life. Most people don't want to admit that, but that is absolutely the way it goes every time. And the only outcome usually being, we're going to start stacking the medications as they start working less and less. However, they were given the second option, which was you can go through some dietary counseling or coaching. And the dietary coaching was so simple. It was not the moronic advice of eat less, exercise more, which just fails. It's because of the caloric paradigm. Calories matter, thermodynamics matter, and this is a guy who got his PhD in bioenergetics.
I have a unique appreciation for energy within an organism. Even still that, that doesn't end up working long term for various reasons, but they were given the advice. Don't count your calories, just control your carbohydrates, prioritize protein and don't fear fat. Especially the fat that comes with that protein. That is the three pillars of the advice these 11 women with type 2 diabetes were given. And then they after 90 days, all the same clinical assessments that had been used originally to confirm their type 2 diabetes, myriad pillars. cardio metabolic markers. Every single one of them had improved. Where at this point now, 90 days later with never a pill popped, never a drug injected, they had no evidence of type two diabetes. Thus absolutely providing even more evidence because there's already substantial evidence for those who want to see it, that type two diabetes and the preceding Insulin resistance is entirely a disorder of lifestyle and primarily nutrition. The food we eat is the culprit or the cure
SHAWN STEVENSON: This is phenomenal, this is and it's so crazy Not very long ago. It was considered just a lifetime disease type two diabetes, once you have it, it's just gonna just be a continuous decline. And as you mentioned, I'm so glad that you said this because we don't say this enough. Most folks don't realize, although this is the fact, once you get on insulin, once you decide that's your course, once you jump onto metformin or now ozempic, this is a lifetime investment. This is a lifetime dedication to taking this drug. Unless somebody comes across. Someone like yourself and if you could you gave us a little bit of a glimpse into Insulin resistance to start this off, but I want to unpack this even more because there's a great Framing that you provided in the book.
And by the way, I've got how not to get sick out right now. It's out today All right.
So Dr. Ben Bikman, along with my friend, Diana Coolian, and you said that insulin resistance if we were to look at this in a more rational, holistic way. It's really there's two sides of the same metabolic coin. All right. So I want to dig in a little bit more on those two sides.
DR. BENJAMIN BIKMAN: Yeah. Yeah. So you, I love that you invoke the coin metaphor. I do that very readily. So there are two parts to this pathology that we call insulin resistance. Most people only consider the first one but I've already alluded to the second. So just to sum them, to bring them both together now. The first problem of insulin resistance is the namesake here, which is that the hormone insulin isn't working particularly well. Now, what is so important, though, is that the audience understands that does not imply that it is a universal phenomenon throughout the entire body.
That there are so many different types of cells, that some cells are still responding to insulin, but some aren't. Now, what's so important, then, this underlying context is to understand that literally, every single cell of the body responds to the hormone insulin. That's not common. Most peptide hormones, which is the family of hormone that insulin is in, do not have a universal effect. Insulin is in rare company where it affects literally every single cell of the body. And I don't use the term literally too liberally like the college kids do these days. It literally affects every cell of the body from brain cells to bone cells, lung cells to liver cells and everything in between.
So again, insulin isn't working particularly well. Some cells, it's less responsive. It's a little deaf to the signal. Some cells hear the signal perfectly well. That becomes a problem when we flip that metabolic coin over and look at the other side, which is the chronically elevated insulin. There is no instance of insulin resistance without the hormone insulin being elevated. You cannot pull the two apart. It's as silly as trying to pull the two sides of a coin apart. You cannot, they always come together. Now that matters because there are, remember, there are some cells that are still as sensitive to insulin as they ever were. And now they're getting overstimulated. A perfect example of the two sides of this coin is evident with the two types, the two primary forms of infertility in men and women.
And just because it's such an interesting example, I feel compelled to mention it. The most common form of infertility in men is erectile dysfunction. Most people don't appreciate that erectile dysfunction is possibly one of the earliest manifestations of insulin resistance in that man, because insulin, one of its many effects on the body, is to induce a degree of vasodilation. It wants the blood vessels to open up. In various parts of the body, including for erectile function, however, as the blood vessel becomes insulin resistant now, even though insulin is coming to those blood vessel cells and telling the blood vessel, Hey, it's time to dilate the signal isn't working.
And so the blood vessel stays constricted and now the man has this manifestation of the insulin resistance as erectile dysfunction. In contrast, the most common form of infertility in females is polycystic ovary syndrome, PCOS. In PCOS, most people don't appreciate that insulin has a mild capacity to inhibit the creation of estrogens. Even further, most people are unaware of the fact that every estrogen in men and women comes from testosterone. So the testosterone gets converted into estrogens. Insulin inhibits that process. So now in a woman, Who has insulin resistance. Those cells of her ovaries maintain perfect insulin sensitivity. So now all of the high insulin, what's called the hyperinsulinemia in her body is acting too much. And it's inhibiting that sex hormone conversion.
And so now she ends up with too much testosterone, but too little estrogens and you have to have a big estrogen surge in order to have a normal ovulation cycle. Normal, very active ovulation requires a big surge in estrogens. She doesn't get it. Thus she fails to ovulate. Thus she has PCOS. So even something like infertility, which isn't lethal, but it's certainly terrible, tragic and inconvenient. We even then see a profound metabolic relevance to this disorder.
SHAWN STEVENSON: Wow. I'm so glad you brought this up. I didn't know we're going to talk about this because, this is one of the, from my perspective, and I think if we were, any of us were just paying attention, this is one of the scariest things about our current time, which is infertility has skyrocketed. There was a great report in the scientific American, we'll put that up for everybody to see, but they were establishing based on erectile dysfunction, based on miscarriages, based on reductions in testosterone. The list goes on and on. They're looking at all these different factors in fertility and they were estimating that fertility is going down like around 1 percent a year the past 40 years.
And so it's pretty scary. And at the root of this, again, we're looking at insulin resistance. And so what I'm hearing is that this is a precondition for so many other things. We tend to just ignorantly connected to diabetes and then that's the end of the story, but it's connected to so much about us and our physiology and that process you mentioned. And again, I'm glad that you brought this up as well. And things starting off as estrogens and getting converted to testosterone, for example, and just having this process like aromatization, for example, and how that can be influenced. By our consumption primarily, I know that this is one of the things we're going to talk about, which is how are we elevating insulin through our diet. But if we could, let's talk a little bit about it because we have to have both if we're addressing both sides of the coin.
We have to have an improvement in that compromised insulin action on the cells number one, and we also have to address and reduce that chronically elevated Insulin level as well. So we've got to do both of those things.
So I want to talk about How do we do both? And in particular, if we're talking about something like having elevated insulin, excessive stress, inflammation. These being the drivers from my perspective, and also, of course, reading your work and analyzing your studies. These being the drivers of insulin resistance, right? We might think about diet. But we don't think about stress. We don't think about inflammation and diet is a part of both of those.
DR. BENJAMIN BIKMAN: Yeah. Shawn, you just pitched several slow balls to me, so I'm going to hit them all out of the park. So watch me hold, don't hold me back here for just a few minutes. Yeah, you mentioned the three, what I consider to be primary causes of insulin resistance. And I use the term primary very carefully and deliberately because there are other causes or other contributors of insulin resistance. Yeah. But they don't meet my standards of being called primary. So there are secondary causes, which for the sake of time, we won't get into.
So the primary causes, which are by my standards, stimuli that are capable of causing insulin resistance on their own. So independent of any other signal. and have also been shown to cause insulin resistance in every biomedical model used in science. So in isolated cells growing in a little Petri dish in laboratory rodents and in humans. The top of all creation, we go all the way through this and we can see that these three things will cause insulin resistance. And you just mentioned all of them, stress, inflammation, and then insulin itself. So to the astute listener, they can already start to see a bit of a vicious cycle that can be created here. And in fact, I'll end on that one just as I cover these briefly. So the first one I'd mentioned is stress. I define stress by an elevation in the prototypical stress hormones.
Those stress hormones are adrenaline and cortisol. In both instances, if you increase either of those hormones, they start to really want to push up blood glucose. That's the one thing they have in common. Cortisol and stress are very cortisol. And adrenaline rather are very different hormones. They have practically nothing in common except they really want to increase blood sugar levels. That puts them at odds with insulin, whose most famous job is to lower blood glucose levels. And so the more those stress hormones are creating an upward pressure on the glucose in the blood the harder insulin has to work to bring it down.
Thus, it's no surprise that they cause insulin resistance. I believe the most relevant variable then when it comes to stress is sleep. Actually, even one bad night of sleep. can cause quantifiable, demonstrable insulin resistance the next day. Very well established. So I focus on sleep as the most relevant variable when it comes to stress induced insulin resistance. And then just moving on to inflammation, any time immune signals are up in the body, And this is most obvious with things called cytokines.
Cytokines are basically little pro-inflammatory proteins. These little, almost like a pro inflammatory hormone coming from the white blood cells, macrophages, for example, are releasing a lot of these cytokines, but a lot of other cells can too, like fat cells, when they get too big, they can contribute to this increased inflammation.
So anytime inflammation starts to go up. It directly causes insulin resistance throughout the body. And in most instances, I believe that's primarily relevant because of a food sensitivity, as well as fat cells that are too big. And that's a conversation all on its own. Why do fat cells get big? And it's a combination of insulin and calories, but then mentioning insulin brings me to the third point. And I end with this point because I do believe it's the most relevant, which is chronically elevated insulin is a cause of insulin resistance. It's, in fact, the one that I believe is the most powerful and prominent of all of the variables. And this is why my approach generally to resolving insulin resistance starts with this heavy scrutiny of carbohydrates, because we have three macronutrients in our diet.
Just to put things in perspective for people so they can appreciate how relevant this is, because I could imagine someone listening, thinking my insulin isn't elevated all the time. Let me just it suggests to the audience just how wrong that view is at a global level. So we have three macronutrients, the three things that we eat, proteins, fats, and carbohydrates. Fat has no effect on insulin. If you and I were to eat a stick of butter and we measured our insulin for three hours, I've done this kind of study, not with butter, but with oil, with olive oil. There is no effect on insulin. It's an absolute flat line. If we did the same by eating pure protein, maybe we get a little bit of an effect.
Some people have a higher effect. Some people have none. It's going to be, I guess we'll say little to no effect with pure protein. Then when we eat pure carbohydrate now, buckle up insulin is going to go up by 10 to 20 times and it's going to be up for about three hours. And this isn't a healthy insulin sensitive person. This is in a college aged male. Who's healthy? This is the most metabolically sound person. Person among the entire population takes a 20 year old man. That guy can handle all kinds of metabolic abuse and shrug it off And yet even in his body give him about 50 to 70 grams of 75 grams of glucose It's going to take him three hours to clear it and his insulin would have gone up.
10 to 20 times now, however If we take the average adult, which is insulin resistant, it's going to take them up to five hours to clear that glucose and eating 50 grams of glucose. That's pretty easy. And you don't even have to, you don't have to bat an eyelash at that. And you already found you've eaten it. Even still, if you take that young, metabolically bulletproof 20 year old man, and give him about three to 400 grams of carbohydrate of glucose, which again is not hard to do. It's very easy to drink or eat that much.
Even in his body, his insulin is going to be elevated for 10 hours, 10 hours. So now let's just take that information and put it in the context of a standard, I was going to say standard American diet, but the more accurate term is a global diet because globally 71 percent of all calories come from starches and sugars. So they're carbohydrates, 71 percent of all the calories we eat at a global level. And when you look even more microscopically, we've been told to eat six times a day. And so you take someone who's eating six times a day, including an evening snack and 71 percentish of what they're eating is coming from carbohydrate.
Everything starts to become clear, where the moment a person wakes up, maybe finally when they've woken up, their insulin has finally come down overnight. It's been working hard overnight and they finally get to a kind of fasted level. And then what do they do? They immediately spike it by drinking and eating refined, starchy, sugary food. And then the insulin has peaked within about 30, 45 minutes to an hour. Right as it wants to start coming down, maybe two hours in, they, of course, have a mid morning snack, and they bump it back up, and then their lunch, and their afternoon snack, supper, evening snack, and so every waking moment is spent in the state of elevated insulin.
And depending on what you eat before you go to bed, and let's face it, most people don't eat protein and fat. They want something salty and crunchy or sweet and gooey. So it's going to be some refined carbohydrate coming from a bag or a box with a barcode. And thus they go to bed having just dumped in a protein. A hundred or 200 more grams of glucose into their bloodstream and now insulin is elevated for hours while they're sleeping. And one final note on this, if you go to bed hyperglycemic, you activate your sympathetic nervous system. You're actually spiking your adrenaline right before you go to bed. So there are a lot of people who blame their insomnia on their anxiety.
And they wonder why they're so hot. Their heart is pounding. They wonder what they're anxious about. You're not anxious about anything. You just spiked your blood sugar, which activates your sympathetic nervous system. So good luck sleeping well. Now you're going to have higher cortisol tomorrow because of your poor night of sleep and you just keep feeding the metabolic beast and thus It's no, it's little wonder why insulin resistance has become the single most common health disorder worldwide.
SHAWN STEVENSON: Wow. This is the vicious circle that so many of us are trapped in and we don't realize it. We're not even giving our bodies a shot to let insulin come down.
Got a quick break coming up. We'll be right back. It's time to get your metabolic oil changed. There's a specific oil that's been found to positively Alter your metabolism. And researchers at Yale university published data reporting that medium chain triglycerides MCTs can readily cross the blood brain barrier and be utilized by our brain cells. So this translates to more energy, but also MCTs are absorbed more easily by other cells of our bodies as well. Medium chain triglycerides are smaller so they can permeate our cell membranes and don't require the use of special enzymes in order for our bodies to utilize The result is more efficient energy. They're also supportive of a healthy gut environment, especially since they have the capacity to combat harmful bacteria, viruses, fungi, and parasites. MCTs are a metabolic and cognitive win, but the quality matters. Make sure that you're sourcing your MCT oil from the very best place. I've been utilizing the MCT oil from Onit for many years.
It's exclusively coconut based. So there's no other nefarious oils that are involved in getting these MCTs. I highly recommend you checking them out. You can add it to your teas, to your smoothies, to your hot chocolates, coffee, and some folks even utilize it for salad dressings, but make sure to utilize these MCTs for better cognitive function and metabolic health. Go to onit.com/model. That's O N I T.com/model for 10 percent off their incredible MCT oil and you get 10 percent off store wide. So make sure to check them out. Go to onit.com/model for 10 percent off. And now back to the show.
SHAWN STEVENSON: You mentioned that this is. One of the, if not the fastest way to throw ourselves into at least a stint of insulin resistance. Do you know what the mechanism is behind that? Why is sleep so important when it comes to our insulin sensitivity?
DR. BENJAMIN BIKMAN: Yeah I can only view it through the lens of the hormone. It's very of hormones. It's entirely possible There are myriad other signals that are contributing but even something like Melatonin improves insulin sensitivity. Dopamine improves insulin sensitivity and I'd already mentioned cortisol and adrenaline, of course. So cortisol is the main signal here, which is, I believe the most evidence really supports the role of cortisol. Cortisol has a natural rhythm to it, as so many hormones do, insulin included, albeit much more subtle than cortisol, which is enormous. Cortisol generally will experience its main bump at around 4 a. m. or so, that latter part of the morning, which makes sense because as cortisol comes up, as everyone remembers, it's one of its main effects.
In fact, arguably its main effect is to increase blood glucose and that does not make it a villain. I don't want someone to hear me and then conclude that cortisol is an enemy. In fact, there are people who have a genetic disorder, they have an autoimmune destruction of that part of their adrenal glands and they can't make cortisol. It's a lethal problem. Cortisol is part of the whole and we need it. It's there for a reason. And even it's, Increase in the latter part of our sleep cycle is important, and the reason why could be that as we're about to wake up in a few hours, it's the body's way of saying, Hey, I'm My brain and the body's about to get a lot busier in a couple hours.
Let's start to increase blood glucose So we're ready to get up and start moving, the brain comes back online the muscles which are the main consumers of blood glucose. We're about to get up. We're gonna stretch. We're gonna start walking around the house a little bit. That's going to immediately increase our metabolic demand and so it's a pretty clever mechanism that the body has devised in order to say, Hey, I'm anticipating a signal, a metabolic demand in a bit.
So cortisol is going to help us as a collective whole meet that metabolic demand. So it's playing its part. However, when you sleep very poorly, that is a signal that ends up amplifying that cortisol signal. So we've turned up what should have been dialed up to a, say a two or three is now dialed up to a seven or eight. And so we've just compounded what was a quiet little circadian rhythm has now become a really big signal. Like we have a metabolic earthquake and that just tells the liver to just keep pumping out glucose like gangbusters. And thus it's no surprise that If we actually clinically measure insulin sensitivity after a night of bad sleep, it is vastly increased.
SHAWN STEVENSON: I'm sending this episode to people. I'm directly thinking about certain people who exercise all the time. They watch their, what they're eating and they're wondering why they're pre diabetic and they consistently are sleep deprived. All right. And you know who I'm talking to. All right. So this is so important because it's an, it's a part of this conversation that is unfortunately left out. And so we can do so much right when we're up and walking around, but if you're not minding your sleep quality and investing in that, making it a priority, you're just going to be continuing to kick yourself right into insulin resistance. And so with this being said, and there's, by the way, there's a great book out there.
It's called Sleep Smarter that has 21 clinically proven strategies to improve your sleep quality, written by yours truly. And, but with that being said, so minding our sleep quality, yes. But there are a ton of folks, what we have today, we have the most sedentary culture that's ever existed in human history. Let's talk about the role of exercise in, in relationship to improving our insulin sensitivity.
DR. BENJAMIN BIKMAN: Yeah, I'm thrilled you brought that up. So as much as I focus on diet as the first step, there's no questioning the relevance of exercise and just moving the muscles. Muscles matter most when it comes to controlling glucose. So when someone eats carbohydrates, If you were wearing a CGM, anyone who's wearing a continuous glucose monitor, and I'm an enormous advocate of their use and continue to be thrilled as more and more people get them and experiment with them when we see our blood glucose levels go up and then it starts to come down 80% of that drop as the blood glucose comes down is because of what the muscle is consuming.
The muscle is just a metabolic hog. It wants all the energy it can get. I joke when I teach these principles and as a professor, that muscle is like the whiny little kid. Okay, the selfish little kid in the family who just keeps demanding once it receives something, it will never give it up metabolically. The muscle is going to hold on to any energy it can get its hands on, and it always wants more, and that's just in part because of the massive muscle we have most of what we're made of. Even in someone who's a little chubby, most of their tissue mass is muscle. Then when you combine that with the fact that muscle can have a high metabolic rate as it gets up and starts moving the body around. It's no surprise that it eats the lion's share of blood glucose.
Now, to make this a little more nuanced, muscle has on it, these glucose transporters. So these doors that will allow glucose to come in that are what's called insulin dependent. So when insulin comes and knocks on the door of the muscle cell, one of its effects is going to be to tell the muscle cell, Hey, it's time to open those glucose doors and let all of this blood glucose come in and feed you. And so an insulin sensitive muscle will do that very well. Of course, if the muscle is insulin resistant, insulin comes and knocks on the door and says, Hey, it's time to open the glucose doors, but the muscle doesn't listen. It's not getting that signal. This is one of the reasons why if someone is insulin resistant and they take in a load of glucose or refined starches and sugars, their glucose levels go high so much and they stay high for so much longer.
It's primarily because the muscle isn't getting the signal very well. Now, lest someone who's listening to this get discouraged and say then what's the point of exercising when a muscle exercises, it becomes so demanding. that it doesn't wait for insulin to give it the signal. So an exercising muscle that is moving in and out, in fact, it's due partly to this, the kinetics of the calcium ion within muscle. There's a huge change in calcium levels. And then calcium basically is able to, through some enzymes, kick those doors open. even without insulin knocking. So there's a back door, if you will, here, where a back channel to open those same doors. So that the working muscle has an insulin independent ability to pull in glucose.
It is, as I said, Basically the muscles' way of saying, Hey, I'm so hungry right now as I'm exercising that I don't have time to wait for insulin. And the good news then to the person who's insulin resistant is that this is an immediate way to start controlling blood sugar levels. Even acutely, if someone eats something that's starchy or sugary, if you just sit down on the couch and turn on a show. You're going to have the whole metabolic storm that you just were flirting with. If you, however, just go on a light 20 minute walk, your muscles have gobbled all of that up and you can bring that glucose spike down by half. It is an enormous reduction. And that's just all because the muscle says and all without the need of insulin to spike.
So I just got done going on and on about the dangers of chronically elevated insulin. This is an instance where the insulin stays low. And the muscle still gets fed and starts clearing all of that blood glucose, allowing the blood glucose to come down, which just enables insulin to stay lower for longer. And the longer insulin is at a low level, the more rapidly the body becomes insulin sensitive so that is why this is a drum that I beat so loudly because it works so well. And then a person may be wondering what's the best way to do it? What's the best exercise? My kind of cheeky response to that is the one you'll do because, if you and I were to tell someone, look, go do CrossFit and we're talking to a 65 year old grandma, she's going to say you can, get out of my house.
I'm not going to, I'm not going to do CrossFit, but if you tell her, Hey, just go on a walk around the block with your girlfriends, she'll do that. So, what the best exercise is the one you'll do. Now, if an individual is capable. Minute for minute resistance training is going to yield better metabolic benefits. It's going to improve the body's insulin sensitivity more than aerobic training will. Thus, I personally am a much stronger advocate of resistance training. It's muscle mass that improves insulin sensitivity. The most incident coincidentally, it's also muscle mass that predicts longevity the best. It's not VO2 max or resting heart rate or these other kind of markers of aerobic fitness. It's muscle that matters. So anything you can do to help build muscle, always try, always default to that one first.
SHAWN STEVENSON: Awesome. If I was to gamify what you just shared, using our muscles is like a cheat code in healing our metabolism and improving our insulin sensitivity. So the big takeaway for everybody, muscle is the number one organ for clearing glucose. All right, so that's number one. And to pivot into another aspect of our metabolism. All right. So you said 80% of that glucose and I would imagine this is going to depend on if we're using our muscles or not too. But optimally 80 but then there are these other types of cells That can gobble up glucose as well and in our society. We tend to fill these cells up a lot more than They might be designed to, but they're very capable and these are our fat cells and you shared that our fat cells can expand their size. They can get so much bigger. They can get about 10 times their size. And if you could, because when we think about muscle, when I hear the word hypertrophy, I think of muscle.
DR. BENJAMIN BIKMAN: Yeah.
SHAWN STEVENSON: But we also have this phenomenon with your fat cells as well. Let's talk about that.
DR. BENJAMIN BIKMAN: Oh, my pleasure. Yeah. This is a topic I love discussing. Yeah. In fact, as much as you teed this up really well, as much as we invoke the term hypertrophy to refer to muscle growth, man, hypertrophy of the muscle can't even hold a candle to the hypertrophy that the fat cell is capable of it. As you mentioned, 10, even 20 times by volume, you can take a fat cell and expand it by that much. There's no cell in the body. that is capable of that degree of hypertrophy. So anytime someone thinks hypertrophy, they should think of the fat cell first just because of its capacity to grow. And this touches on another cause of insulin resistance.
So earlier I'd mentioned the three primary causes. Those are capable of causing insulin resistance like acutely within hours. You spike cortisol, that person, that cell is insulin resistant within just hours. Same with insulin. If insulin goes up for just a handful of hours, the body's already starting to reduce the signal, becoming a little insulin resistant. So those are rapid causes. They're also rapid resolution. Now, over time, however, we have a more chronic insidious kind of insulin resistance. It takes longer to improve. And this is when the fat cell becomes important. And what's so interesting about fat mass is that we focus on the mass of fat, but it's the size of the fat cell that matters most.
So in other words this explains why Someone could go to the liposuction clinic and have immediately 20 pounds of fat removed from their body. And before they had this, they could go in and get every cardiometabolic marker measured. And I talk a lot about them, by the way, and how not to get sick. The whole first chapter is looking at all these metabolic and cardiometabolic markers to determine someone's insulin resistance. They could get all of these markers measured. Go in, get 20 pounds sucked out of their body of pure fat. And if it was only if metabolic health was purely a matter of the amount of fat a body had, you would think every marker must be improved.
And yet not one is better. So following liposuction, not one single marker is improved because it's not the mass of fat that matters most. It's the size of each fat cell that matters most. And there's some fascinating differences across ethnicities. I, for example, did my postdoctoral fellowship. So after a PhD, if you want to become an academic scientist, you have to do a fellowship period. I did my fellowship with Duke medical school in Singapore, this beautiful country in Southeast Asia. We love it. It's a second home. One of my kids was born there. We love Singapore, but Singapore was interested in understanding across their the populations within Singapore. Why is it that a chubby white guy is perfectly fine? And yet a chubby Chinese Singaporean already has fatty liver disease. He has hypertension. He has type two diabetes. And even though they have the exact same amount of fat on their bodies just as a point of interest, if you want to be really fat, you want to be Caucasian. White people can handle the most amount of fat on their bodies. On the other end, is Asians and South Asians or Indian, Asian, Indian. They have the lowest tolerance for body fat. And that's because their fat cells get very big, very early because they have generally fewer fat cells on the body.
And so this brings me to the point then, what is it about the hypertrophic fat cell that matters so much? It's two things. First thing, and this will blow some minds, you cannot have a fat cell grow unless insulin is elevated. It is totally, completely, utterly impossible. Now, I know people want to say, oh calories matter too. They do matter, but if you just take out that one single variable. If you deprive a fat cell of insulin, it can not grow. 100 percent full stop.
Take this as from a guy who literally grows fat cells in my lab all the time. In a human model, you even see this. If you have a person with type one diabetes, They can eat 10, 000 calories in a day and all they do is skip an insulin injection and they will be as skinny as they want. In fact, this is so well known to that diabetic that it's a known eating disorder. It's more of a hormone disorder. But if they just skip their insulin injection, they'll be as skinny as they want. It's a condition called diabulimia. You only eliminate one single variable, the insulin. They not only grow fat, they can't even hold on to it. So as much as calories matter and they do. Insulin is an absolutely necessary signal to tell the fat cell to grow and then the calories help fuel that growth.
Now that was a bit of a tangent, but so let's come back to the hypertrophic fat cell. So you have a fat cell that's getting, I promise it, matters because as the fat cell starts to get so big, it's like a water balloon that's getting to the point of maximum growth. And if you continue to put water in that balloon, it's going to pop. And so as insulin is high and there's sufficient calories to fuel the growth that the insulin wants the fat cell to, to undergo, the fat cell starts to tell insulin, you continue to make me grow. But I can't grow anymore, so I'm going to stop listening to you. And so the fat cell that's grown so much becomes insulin resistant to stop growing.
So it's a survival mechanism. The poor fat cell is literally, if it continues to grow, the membrane cannot hold it together. And it will start to fragment and literally start to pop, which will be very unhealthy, cause a lot of inflammation. And there'll be a messy process in that fat tissue to try to clean up. Very unhealthy. So the fat cell becomes insulin resistant to stop further growth. Number two, as the fat cell gets bigger and bigger, it starts to get pushed further and further away from the capillaries, which is the main blood vessel where the blood is giving up its oxygen and giving up its nutrition to a cell and taking all of the waste products away from a cell.
So if a cell is getting pushed too far from a capillary, it starts to suffocate. The technical term at the level of the cell is it starts to experience hypoxia. It becomes hypoxic. And if the cell doesn't get sufficient oxygen, Once again, it will die. It will be a very messy process and we don't want ourselves to die. And the fat cell doesn't want to die. And so it starts leaking out these pro inflammatory cytokines. This word I mentioned earlier, some of those cytokines kind of act like a trail of breadcrumbs where when the capillary senses those breadcrumbs, it can follow them back and start growing a new blood to feed that suffocating fat cell.
So the fat cell has another mechanism to ensure its own survival, to correct its hypoxia in this case. But in the process, it is now leaking all of these pro inflammatory cytokines throughout the entire body, causing what we commonly call subclinical chronic inflammation. So it's not like their inflammation has reached the point of an autoimmune disease or a cold or flu, but it's higher than it should be in someone who's otherwise healthy. And it's all because of the hypertrophic fat cell. And so we have high insulin and the insulin resistance as the fat cell tries to stop growing. And then we have the inflammation as the fat cell tries to correct its hypoxia, both of which just contribute to insulin resistance throughout the body.
So I generally say the fat cells, the first. Domino to fall. And then when the fat cell becomes insulin resistant, it's promoting this insulin resistance to other tissues like the liver, like the muscle, like the brain, causing fatty liver disease, causing sarcopenia or wasting of the muscle or causing Alzheimer's or migraines or depression, in the case of the brain.
SHAWN STEVENSON: You're detailing why obesity is a primary comorbidity for Alzheimer's, for cardiovascular disease, for thyroid dysfunction, for autoimmune diseases. The list goes on and on. You're detailing for us why that is, and it's really rooted in that inflammatory cascade. So what I'm hearing is that our fat cells are even giving us warning signs when they're starting that process with hypoxia, for example. Before we even get to that place of them popping, which is that extreme scenario, our body is giving us feedback. It's an adaptation. So it's sending out all this kind of a distress signal in a way.
DR. BENJAMIN BIKMAN: Absolutely. That's the exact what that's how exactly I refer to it. The poor fat cell is just trying to survive. And it's like firing up these flares that we unfortunately just don't have a clinical system in place to detect it.
SHAWN STEVENSON: Oh man, this is so powerful. All right. I've got to ask you about this because one of the things you've mentioned this, and I'm so grateful that you've done this, you keep bringing calories back into the conversation. But providing the context because it's calories plus context we can shovel in calories all day all night and we're not going to expand our fat cells or store this if insulin is not present. We cannot leave our hormones out of this conversation about calories. It's just ignorant. And so, with that being said, we've got the power of exercise that you already mentioned, and it really being a cheat code to helping to heal our metabolism, to help us to clear blood glucose. And you mentioned, this is so crazy.
This is our first time talking, and there's so many similarities because I've said this for years, and this is, we can go back in the track record and listen to shows from 10 years ago. My favorite form of exercise for people that I was working with is a form of exercise that you'll actually do. All right. I've said that so many times now with this being said also in knowing being able to work with so many people over the years Knowing a little bit about human psychology, we love ease, if we make things too complicated, it's more and more reasons for us to not do a thing or for us to say, I'll get to it later.
And so one of the great things about this book, and again, this is available right now. And it's a, first of all, it's beautiful. It's a beautiful book. All right. How not to get sick is available everywhere books are sold. So you've got this incredible knowledge just packed in you literally just packed it into the beginning portion of the book. And then we have Diana Coolian who's showing us simple little to no equipment strength training exercises to really extract maximum benefit without a lot of fuss without the need to run off to go to a gym which again, if you love going to the gym. Keep doing that. That's awesome. But For many people it's just that ease of access and to know exactly what to do. So you have your own personal trainer to walk you through these different exercises and again, it's laid out so beautifully. She describes the stuff in a very poignant simple way and then you get to the recipes as well, and it's all backed by science the way that you guys structure these recipes. And so, before we get into the collaboration and how that unfolded and turned into this beautiful project.
The one thing that jumped out that really spoke to my heart when reading this book was how neglected insulin is in the conversation about metabolic health. Now, again, it's not that we're not talking about it, but we're missing the context. If we're looking at it through the lens of, We're obsessed today, and that's great that we are, it's a part of the equation, with tracking blood sugar, and hemoglobin A1c, alright? These are important markers when talking about insulin resistance. But, it's so crazy, and you're giving the tests, in the book, here's the test to do, and That we're not tracking insulin sensitivity. We're not tracking insulin itself. And you talk about some of the tests that people can do, including a fasting insulin, right? So we're looking at part of the equation with blood sugar, but if you're not looking at what insulin is doing, then you're going to be missing out on the full picture.
DR. BENJAMIN BIKMAN: Yeah. Yeah. Yeah, just that is probably, in fact, Shawn, if I had to say, if someone asked Ben at the end of your career, what is one thing you hope you've accomplished? This is it. My hope is that in some way, I may have had some contribution, albeit modest, if only, to changing the clinical paradigm of metabolic health, and not excluding glucose based markers, but just saying, that's not the hero. That's not the main character of glucose in any glucose related marker, like glycation of hemoglobin, HbA1c.
It's the sidekick. It's the Robin to the Batman and insulin is the main character here. It is the main metabolic marker. It absolutely matters most. Thankfully, it can be measured at every single blood test. We just have both what I consider to be a scientific and a historic precedent that has left it out. Those should not be barriers anymore. Any lab, anytime you're getting your blood drawn, you can ask that person, ask that physician, ask that nurse, the PA, whoever it is, say, Hey, can you just check this out? that box and measure my insulin to they may not know why you want it measured, probably because they never were taught why it matters.
It's you only know what you've been taught, but insulin is going to be the early signal. And this is why, if everyone who can please get your fasting insulin measured, once you have your fasting insulin, That alone has a diagnostic value and then you can start to combine it with a glucose with your glucose marker and create a whole new marker called your HOMA, H O M A score, which itself becomes a very valuable marker of insulin resistance. So we have the technology, we have the means. At this point, it is purely a lack of education. But even, Shawn, what's funny? As much as we're talking about insulin resistance, most people still don't really appreciate it. Like when I wrote my first book, the reason I didn't call it, what is insulin resistance and why does it matter?
It's because I knew no one would buy it. No one would, everyone looks at the word insulin and immediately just thinks diabetes. They don't realize the relevance of insulin in their own body, in their own life. And we'd been talking about the fat cell and calories. Insulin does so much throughout the entire body. That's why I thought I need a sexier name here. And so that was the birth of the why we get sick title. But yeah, insulin is the marker that matters most. And the more we overlook it, the longer it's going to take us to actually determine the problems.
SHAWN STEVENSON: Now, I want to ask you a little sidebar question, because in just spending time in your world, I came across some great research that you were sharing on, and this is the cool thing about being alive today. We've got thousands of years of humans doing certain things and now we've got science to affirm Oh, it actually does this. And one of these interesting things in regard to metabolic health is cold water immersion.
DR. BENJAMIN BIKMAN: Yeah.
SHAWN STEVENSON: All right. So can you talk a little bit about that? Why You decided to look into that more and some of the metabolic benefits that we can extract from that.
DR. BENJAMIN BIKMAN: Yeah. Yeah. So I'm an enormous advocate of these contrasting therapies that get into the realm of hormesis. So hormesis is a term of physiology that refers to something that can be beneficial within a range. and perceived as harmful and indeed can be if it's too much. So it's this kind of hormetic stress. This idea that a little bit of shock to the system is really good exercise is a hormetic stress fasting. And then we have the temperature extreme sauna, which I also love. And then cold immersion or cold exposure, which I also love. I like both of those extremes and this may be partly because I lived in Russia in the mid nineties and I got used to that kind of Russian.
What's called the Banya when I lived there for a couple of years. And, you have this sort of very Finnish style of sauna where you're sweating your guts out with the boys. And then you go literally roll in the snow or go into a cold pond where they've chipped the ice away. Then you go back into the sauna and I just fell in love with that process. So cold therapy, cold immersion, there is, there are multiple signals that come in to improve metabolic health. The most obvious is the shivering. So shivering induced thermogenesis is an immediate effect where every time you're shivering to try to generate body heat, you are consuming glucose.
That's like a little form of exercise where you're just rapidly starting to pull in glucose and that allows insulin to take a break. But what is much more subtle, but more lingering than the shivering, even long after you stopped shivering, you will have a lingering effect of having activated a type of fat called brown adipose tissue or brown fat. So it's a little known fact that within humans and many other animals too. The majority of the fat we have is white fat. So if we actually look at the fat, if we pulled a piece of fat out of that person's belly, and I do this in my lab here at BYU, it's very white. It has, it's very loaded with fat. It almost looks like Crisco.
It has a very low metabolic rate. And we measure metabolic rate in tissues, including fat cells. It's almost below the point of detection. It is such a low metabolic rate. In contrast, humans also have, and other animals do too, a type of fat on their bodies in certain locations called brown fat. And it is in fact a dark reddish brown. In humans, it's primarily through this what's called thoracic cavity. And if you looked at a piece of that fat, very dark brown, reddish brown, it has a metabolic rate that is comparable to muscle. It is about 10 times higher than the metabolic rate of that, of the white fat. And it exists primarily, if not exclusively to generate body heat.
It is very wasteful in its metabolism. So it's burning glucose and it's burning fat, not because the cell needs energy to contract or send a signal across a neuron, any of the cellular work it burns just to create heat, which chemically is very inefficient, but metabolically very beneficial for someone who has fat that they want to burn.
So brown fat whose primary job is to create heat gets very stimulated with cold therapy, no surprise. In fact, As another point of interest, humans as babies, we have a lot of brown fat, which is an essential compensation while we have very little muscle. So notice anyone who's got a little baby and I've looked at this, observed this with my darling little babies as they've grown. There's a point where if you take the baby out of the bath, the baby isn't shivering, because it's cool. Now, a baby may have little twitching sometimes, but it's not because it's cold. So the baby doesn't shiver to generate heat because baby little humans have a lot of brown fat. So it's like they're little incubators that are just have these fat cells that just ensure the body heat stays at a normal level.
But as we grow up our body fat, especially our brown fat starts to run out and our muscle mass starts to go up. So the primary mechanism of warming a body. in someone who's gone beyond infancy. So a child and beyond is now shivering because we have enough muscle to do it. And so shivering induced thermogenesis became, becomes the main way. But anyway, back to the cold immersion, back to insulin sensitivity, the more these cells are busy trying to warm the body. either through shivering at the muscle or this inefficiency of the mitochondria, to be very specific of the brown fat cells. Just the more glucose those cells are using, the easier time the body has then bringing glucose down. And then of course, the more glucose is staying low, the more insulin can stay low too. And any time insulin is down, the body's becoming more insulin sensitive.
SHAWN STEVENSON: Amazing. Being a distinguished scientist, Dr. Ben Bickman just shared why cold exposure is so remarkable for our metabolic health. We've got several studies affirming its benefits on improving our sleep quality, on reducing inflammation, on improving the function of our satiety hormones and other metabolic hormones like its influence on insulin sensitivity. The list goes on and on and I get to share with you, recommended by his co author, what the very best cold plunge tub is for you to use. There's one cold plunge tub. That's always ready to use. You don't have to find bags of ice. You don't have to constantly clean it. You don't have to go through all the rigmarole just to be able to get a great cold plunge experience. The original cold plunge tub from plunge has continuous water flow and a 20 micron filter that pulls out debris and keeps your cold plunge tub clean.
It's self contained with no need for additional plumbing. You can utilize it indoors or outdoors. We have ours outdoors and also it's long lasting is durable. The plunge tub is made with an amazing acrylic and fiberglass with a reinforced Metal base that will last you a lifetime. We've had it for a couple of years and it's still like it's brand new. And right now you're going to get $150 off the cold plunge tub of your choice by using the code MODEL150 at checkout. When you go to plunge.com/model, go to plunge.com/model that's P L U N G E.com/model and use the code MODEL150 at checkout to get yourself the very best cold plunge tub in the world.
And by the way, Dr. Bickman also mentioned contrast therapy. So utilizing a sauna and. A cold plunge as well. And guess what? Plunge now has the most amazing saunas available. You've got to see this incredible design. It's going to knock your socks off. So you can check out their saunas there as well. And by the way.
MODEL150 gets you $150 off any sauna of your choice. And so they have these cool flip up benches inside the sauna where you can actually have space to do yoga. What? You can do some stretching. Of course you could seat several people in there as well. And this isn't your typical run of the mill sauna. This is utilizing the best science backed design to generate the heat that you're looking for. And also an ergonomic design that's spacious. There's a high ceiling and it just makes it comfortable. To enjoy your sauna experience. So whether it's getting your cold plunge, whether it's getting a sauna or getting both, plunge is really setting the standard on supporting our metabolic health and making these incredible health resources accessible. And by the way, because this is an investment into your health and longevity. Plunge even has no interest financing options, protection plans, free delivery and other perks. So again, hop over to plunge.com/model, use the code MODEL150 at checkout. And now back to the show.
I love this because this conversation is getting us to think more broadly. It's not just this isolated thing. And you even shared in one of your videos, the influence that it has on thyroid hormone, for example, and so it's just there's so many incredible things. And you just mentioned this practice that's been done in a certain culture for centuries, right. And there's a reason behind it, there's a method to the madness in a way. And, thank you so much for sharing those little insights on that. And. If you could, because this is what we're all here for today, is practical application. We get the knowledge, and also, what do we do with this?
Because we know that our food has a huge impact on our metabolic health, on our insulin sensitivity, and there's a certain way of eating. Right? How not to die and how not to get sick. A certain way of eating that can support this, but also not deprive us of the joy of eating. And that is where Diana comes in as well in your collaboration on this project. What are the principles, the science backed principles, that you provided her with. And by the way, I love you. I got to see this firsthand in her life. All right. I got to see her transformation. I've known her for many years. And before I, I don't, this is long before the book came about, and I saw the things that she was doing.
Like we went out to eat and I just see like her choices. I'm just like, okay, is that right? And before, like she is from her perspective also, she'll share this, like the fittest she's been in her adult life and having a family. Having two kids and doing all the mom's stuff. And she's like getting a degree, another degree in something.
And her changing for hers, that was the biggest on ramp was just changing what she was doing with her nutrition. And there's a certain principle, there are principles behind it. And if you could, can you share the principles behind the recipes that people are going to find and how not to get sick?
DR. BENJAMIN BIKMAN: Yeah, my pleasure. In fact, let me just add to your enthusiasm with Diana. When my publisher first had said. Ben, we need to have a more kind of concrete plan for helping people improve their insulin resistance. I had told them, look, I'm a great teacher. I'm a great professor, but I'm not a great coach. And so I need, I can't make exercise plans. I can't make meals, meal plans. And they said, Oh, we got someone in mind. And the moment I'd connected with Diana, I knew this was a perfect match where I can be the teacher and she can be the doer. I can be the one who provides the principles. She can be the one who provides the plan to implement those principles.
So it really put me in a very comfortable position where I could stay as the scientist and professor, and she could be the person who's done it all and shares all of her experience with it. So the nutrition plan, which Absolutely matters most as much as I'm an advocate of exercise and we lean into that in the book on purpose because it does matter so much. Exercise cannot fully make up for a diet that is not up to code. If your diet is really lagging, exercise is only going to help so much. So it's based on the principles that I mentioned earlier so now but with including a fourth so the first one is control carbs. And we provide a plan depending on where the person is based on those metabolic markers that I start the book with. It puts them into one of three categories where they can either be in a position.
Jealously, they may be in a position to just maintain their insulin sensitivity. One of those few who are very metabolically sound or more likely. There's someone who needs to prevent, maybe they're sliding into insulin resistance and they got to reverse or they're all the way in and now they got to reverse it completely. And so they get, you get put into one of three categories that ends up. Putting you into some different macronutrient mixes and the book, as you noted, it really is elegantly put together, even color coded on pages, depending on which category you put yourself in with regards to your, where you are on the spectrum of insulin sensitivity, but to wrap all of them up. It's focused on control carbs. So it's a heavy focus on the starches that the carbohydrates that have the least impact on glucose and insulin. That is the primary motivator here. How can we keep, how can we nourish the body, but keep glucose and insulin in check. So it's focusing on smart sources of carbohydrate, namely fruits and vegetables. So that's the control carb part of it. And then prioritize protein. And I would say that don't fear fat principles. They really should come together in our fear of fat.
We have pulled the two apart now, Diana, and I don't do that because in nature you never see that there is no such thing as a protein that exists in nature that comes in the Absent fat. In other words, every protein in nature has fat with it, and that is how we should eat it. If you eat protein in isolation, you don't digest it as well. You minimize the anabolic effect of that protein on muscle. This is all evidenced in human studies. When protein comes with fat, we both digest it better.
And it has a stronger anabolic signal than the protein alone. So muscle protein synthesis is stronger when protein is consumed with fat. That's how I advocate people eating it. Whether you want to invoke a divine authority or just nature and evolution, if nature says all proteins come with fat, it stands to reason that the human body is built to bring it in that way. So who are we? to defy evolution or God and pull those two things apart. Keep them together. Protein and fat come together. That's how we should eat them. So prioritize protein and don't fear fat. I could say, don't fear the fact that comes with that protein and it's going to have little to no effect on insulin.
And speaking of nourishment, that is the nourishment that matters most. I'm not an enemy to carbohydrates, but there is no such thing as an essential carbohydrate. Literally, it does not exist. There are such things as essential amino acids. Thankfully, you'll get them all from any animal source protein. There are such things as essential fats. Thankfully, you'll get them all and more from every fat source, every animal source fat. So I'm an advocate of animal sources in those instances, just to ensure you get them all. But again, no essential carb. That doesn't mean don't eat any of them. But it means don't make it the main part of your diet.
Why would we make the main part of our diet? The very one thing that we don't need to focus on the things we need. And then the fourth and final principle is fasting frequently fast. Find a way to incorporate fasting into your daily plan. But my only point on that is how you end your fast matters more than how long you fast. So the food you eat when your fast is over matters much, much more than how long you fast. And I say that born from the abundant experience of seeing people who will go on a 24 or 36, 48 hour fast and then binge, whatever they can shove in their mouth, they shove in their mouth. And then they end up feeling sick.
They feel ashamed. They hate to admit this kind of addiction that they're trying to fight with food. And it ends up becoming a form of fasting bulimia where they're binging and purging, but in a sense of fasting. So they only eat one time a day, but man, it's a bunch of garbage. It's gummy bears, it's candy, it's cakes, it's cookies. No, it'd be better to have a shorter fast and keep those macronutrient rules in mind than have a longer fast and throw the macronutrient rules out the window.
SHAWN STEVENSON: I love that. And you mentioned that in the book as well and how important that is. And again, I don't think a lot of people think about that in the context, obviously fasting different versions of it have become popular today. And even though it's been utilized for thousands of years, even if on accident but. How you're transitioning back into eating is super important because of what is going on with insulin. And so some of these recipes, I can't even begin to tell you. And I love the fact that, again, you mentioned it's color coded for everybody.
But I can't even begin to tell you how delicious these recipes are and how easy they are. She made them very simple as well, and so it doesn't take a lot of work to make so many things. And these are great things to batch is another thing that I noticed as well. So it's a great chili recipe, the Baja fish tacos, the blackberry cheesecake squares, of course. And again, this is just scratching the surface. So many amazing recipes. It's all just laid out for you and in this plan and also again the exercise portion as well All in one source plus the education. You can pick up this book right now All right, head over to Amazon or your favorite bookstore. Get your copy today.
This is an essential guide and again, you are adding to something so important to this conversation that is crazy that has been left out. This education around insulin is so it's a game changer, because you gave us the insight today on why this is impacting multiple epidemics of chronic disease in your book, really enlightening us in particular, in your first book, why we get sick and looking at these multiple epidemics of chronic disease that we have today. Epidemics of Heart disease, cancer, diabetes, Alzheimer's disease is creeping his way into the top five leading causes of disease.
This is rooted in a part of this metabolic health equation that isn't being talked about, or it definitely isn't being talked about enough and to the degree that you are teaching us. And so it's so wonderful, and I'm so grateful that you put this out for us. Can you let everybody know where they can connect with you more, get more information, just get into your universe and also. Shout out to where they could pick up a copy of the book.
DR. BENJAMIN BIKMAN: Yeah. Yeah. Shawn, thanks so much. Really, from the bottom of my heart. When you're a professor who thinks you've got an important lesson to teach, all you want is a bigger classroom and that's what you've been giving me. So I appreciate it. Yes, people can find me, the best way to connect with me and find what I'm doing is my website, insulin IQ. It's a site that I created to really just act as my central platform. All just trying to share this metabolic message of the relevance of insulin resistance, and then you'd mentioned my books, Why we get sick. How not to get sick. Both of those are available anywhere books are sold and it's just more of my efforts to educate.
SHAWN STEVENSON: Awesome. This has been, I've loved this conversation so much. You have no idea. I've been over here just like fanning out over what you're sharing and how you're sharing it. And just really helping to bring this to life for us, we, all of us learn differently and just being able to really understand the why behind certain things is catalyzing for some people and other folks need to know the how, they just want to know what to do, right? And so having all of that together in one book is super special. And I've got 100 other questions for you. So we're going to have to do this again if you'd be up for it. And just, I appreciate you so much for putting your time and energy into creating this for us. So thank you so much.
DR. BENJAMIN BIKMAN: Oh, my pleasure. My pleasure. Thanks so much, Shawn.
SHAWN STEVENSON: Dr. Ben Bikman, everybody. Thank you so much for tuning into this episode today. I hope that you got a lot of value out of this. Our metabolic health and this education around this subject matter is more important than ever. Please share this out with somebody that you care about, share it out with your friends and family, share it on social media, help get this information into the hands and hearts of more people.
We've got some amazing masterclasses and world class guests coming your way very soon. So make sure to stay tuned. Take care. Have an amazing day. And I'll talk with you soon. And for more after the show, make sure to head over to themodelhealthshow.com. That's where you can find all of the show notes. You can find transcriptions, videos for each episode. And if you've got a comment, you can leave me a comment there as well. And please make sure to head over to iTunes and leave us a rating to let everybody know that the show is awesome. And I appreciate that so much and take care. I promise to keep giving you more powerful, empowering, great content to help you transform your life. Thanks for tuning in.
Maximize Your Energy
Get the Free Checklist: “5 Keys That Could Radically Improve Your Energy Levels and Quality of Life”
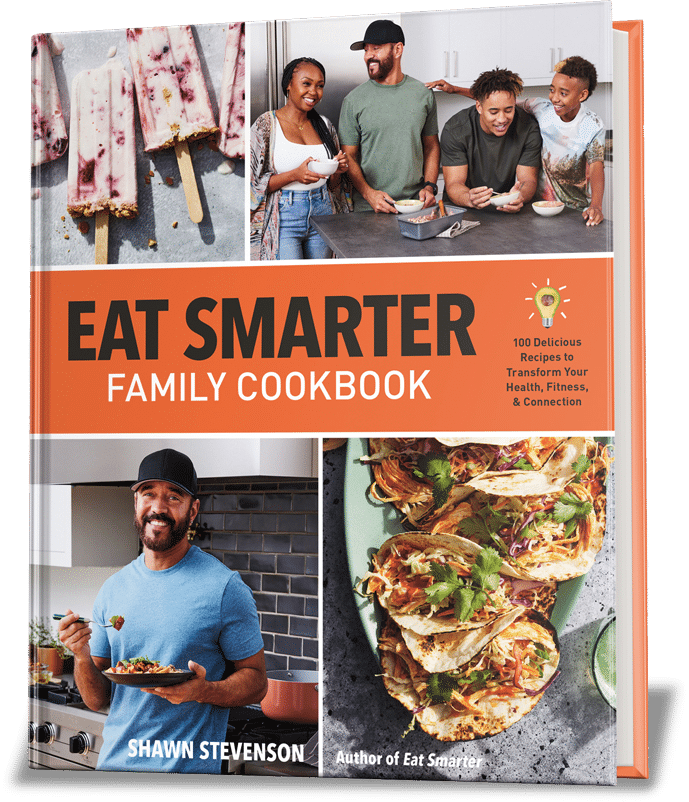
HEALTHY MEALS EVERYONE WILL LOVE
The Greatest Gift You Can Give Your Family is Health
When you gather your family around the table to share nutritious food, you’re not only spending quality time with them - you’re setting them up for success in all areas of their lives.
The Eat Smarter Family Cookbook is filled with 100 delicious recipes, plus the latest science to support the mental, physical and social health of your loved ones.









Share Your Voice
0 comments. Be the first to leave a comment.