Subscribe to The Model Health Show:
TMHS 692: How to Heal Faster from Injuries, Eliminate Pain, & Master Rehab Science – with Dr. Tom Walters
No one is immune from pain and injuries; they’re an inevitable part of life. Luckily, our bodies are incredible in their capacity to heal and recover. But if you want to heal faster and more effectively, having a foundational understanding of pain science can yield incredible results.
Today’s guest, Dr. Tom Walters, is a board-certified orthopedic physical therapist and strength and conditioning specialist. In this interview, he’s sharing principles from his new book, Rehab Science. We’re going to cover exactly how pain is created in the body, how to heal from injuries faster, and the role of the brain and nervous system in managing pain.
You’re going to learn the science behind pain, tips for faster recovery, and the basics of wound healing. Dr. Tom Walters is a true expert in all things physical therapy, and I know you’re going to find his insights valuable. So click play, listen in, and enjoy the show!
In this episode you’ll discover:
- Why pain education is so important.
- The definition of pain.
- How the potential for tissue damage can create pain in the body.
- What nociception is.
- The psychological factors that can influence pain.
- What the biopsychosocial model of physical therapy is.
- How the sensitivity of the nervous system can affect the sensation of pain.
- The truth about immobilizing an injury.
- Why pain and injury recovery require active participation.
- The fascinating link between the immune system and pain sensors.
- What flexion sensitivity is.
- The connection between depression and low back pain.
- Main differences between injury and pain.
- Three basic phases of wound healing.
Items mentioned in this episode include:
- Beekeepersnaturals.com/model — Save 20% on raw honey & other natural remedies!
- PaleoValley.com/model — Use code MODEL for 15% off!
- Rehab Science by Dr. Tom Walters
- Connect with Dr. Tom Walters Website / Instagram / Facebook / YouTube
Thank you so much for checking out this episode of The Model Health Show. If you haven’t done so already, please take a minute and leave a quick rating and review of the show on Apple Podcast by clicking on the link below. It will help us to keep delivering life-changing information for you every week!
Transcript:
SHAWN STEVENSON: Welcome to the Model Health Show. This is fitness and nutrition expert Shawn Stevenson, and I'm so grateful for you tuning in with me today. Pain and injuries are an inevitable part of life. Nobody's making it through this human experience unscathed. Now, here's the thing. We don't often get educated about how to recover from injuries effectively. What does the latest science say?
And also how is our body associating and creating pain in the first place? Is pain simply due to some mechanical insult? Or is there something far more complex at play? If you've been wanting to find a way to get out of pain or to have strategies to help somebody that you care about. Or in particular, having these things in your superhero utility belt to help you to heal and get over pain, to address chronic pain and/or even acute pain when you're injured. If you want to have these strategies there when you need them, which I highly, highly recommend that you do, this episode is for you.
This is going to change the game when helping to understand what pain actually is and how to intelligently recover from injuries and pain whenever life presents its inevitable problems. Now, before we get to our special guest, I want you to keep in mind that it's not just a mechanical insult or some kind of trauma that can trigger pain, and we're going to really deconstruct that on this episode. But stressors of all types can actually trigger and exacerbate pain or even create the circumstances where injuries are more likely. Alright?
So being sleep deprived significantly increases our risk of injury and pain. Also, having stress related to our work or relationship stress. We know about that internal pain from a broken heart, yes, but this can actually create real physical pain.
Now, there's actually broken heart syndrome that's been published in peer-reviewed data and really illuminating something that we talk about just kind of superficially, but it is actually a real phenomenon. Now, that stress can show up in other places besides our heart, obviously. And again, we're really going to dive deep into this, but I want you to keep in mind that poor diet is one of the primary stressors that are causing so much pain and suffering.
We tend to think about it in terms of maybe an acute thing, right? We eat something and then we have "food poisoning" or an upset stomach, our tummies, our tummies are upset, or we think about long-term chronic degenerative diseases caused by our poor diet. Now, we've talked about this many times on the show, but research published in the BMJ found that nearly 60% of the average American adult's diet is now made of ultra-processed foods. And American children, that number is inching it way close to 70% of the average child's diet in the United States is made of ultra-processed foods.
So, we are inherently experiencing food trauma. We're experiencing a food stressor that's causing pain and degeneration within our system. And here's the other thing about food. With fake food causing problems and real food oftentimes presenting a solution. And as you're going to discover on today's episode, part of this pain process and healing from injuries is also reeducating our nervous system. And there are a couple of things that's been discovered that can actually help to heal our nervous system to provide accelerated healing from even injuries, even physical wounds.
One of those storied things is honey. Now many people have heard that honey can actually help to accelerate the healing of wounds and burns. And this has been used for thousands of years for those purposes, it's incredibly effective at that. But also internally, honey can make some huge changes.
A study that was published in evidence-based complementary and alternative medicine found that polyphenols in honey were found to reduce inflammation in the brain, is found to reduce neuroinflammation. And not only that, there were some beneficial side effects, which was improving memory and actually helping to improve cognitive function overall.
Who knew? We think about honey topically for helping to heal wounds, but it can actually help to heal what's happening internally as well when a brain is set on fire. Now, another study that was published in Advanced Biomedical Research found that, again, we know about the power of honey, but what other bee products might be helpful with reeducating our nervous system?
The researchers found that royal jelly, this is what the queen bee exclusively is feeding on. Royal jelly has the potential to improve spatial learning, attention, and memory. And it was found to have specific anti-inflammatory effects in the body and helping to, part of the process we're going to talk about today is due to neuroplasticity.
So Royal jelly's been found to help to differentiate all types of brain cells and help to stimulate neurogenesis in the brain, right? And so obviously the brain, we have the central nervous system and the peripheral nervous system. Royal jelly has been found to be beneficial for all aspects of our nervous system. So again, helping the body potentially to support reassociating, remodeling pain in the body.
Now, when it comes to honey and royal jelly, we really want to focus on regenerative beekeeping because our population of bees has been declining in recent decades because of all the environmental pollutants, deforestation, all of these human interventions are causing a loss of our bee populations and bees are responsible for pollinating so many of our foods. And so truly to take care of ourselves, we need to start taking better care of our bee population.
So, number one, investing in sustainable beekeeping. And number two, making sure that your bee products themselves are not riddled with pesticides and environmental toxicants. And there is one company that's doing third party testing for over 70 pesticide residues commonly found in bee products.
Also, making sure that there are no pervasive offenders like heavy metals or E. Coli or things like DDT that are again, commonly found unfortunately in bee products, making sure that none of that is coming along with these incredible super foods. And this is why I get my royal jelly and I get my Raw Superfood Honey from Beekeeper's Naturals. Go to beekeepersnaturals.com/model and you're going to get 20% off storewide. That's B-E-E-K-E-E-P-E-R-Snaturals.com/model. 20% off their royal jelly is coming in their incredible product called Brain Fuel. It's a nootropic that helps to optimize our cognitive function. It's designed really to improve attention; it's designed to improve our memory.
And one of the other ingredients in there besides royal jelly is one of my other all-time favorite things, bacopa. A randomized double-blind placebo-controlled human trial published in 2016, found that after just six weeks of use, bacopa significantly improved speed of visual information processing, learning rate, memory consolidation, and even decreased anxiety in study participants.
This is as close as it gets to something that's sustainable, time tested if we're talking about a limitless pill. Alright, head over there, check them out. Their Brain Fuel is one of my favorite things. And of course, their Superfood raw honey is a staple in my family's cabinet. Go to beekeepersnaturals.com/model. And now let's get to the Apple Podcast review of the week.
ITUNES REVIEW: Another five-star review titled “Shawn Stevenson Rocks” by Tricks 2022. "Shawn is one of the most knowledgeable, authentic and down to earth health experts out there. I read his books and learned so much about health, nutrition and living my best life. Now I don't miss any of his podcast, which I listen to on long walks with my dogs. Sometimes I listen to an episode a second time when I'm home so I can take notes. His guests are always interesting, and I doubt I would find any of these health experts and their books on my own. Shawn has been making such a positive impact in the world, and I intend to spread the word within my circle of friends."
SHAWN STEVENSON: Wow, this is absolutely incredible. Thank you so much for sharing that over on Apple Podcast and thank you for taking me along with the pups on the walks, and I really do appreciate that so much. And listen, if you yet to do so, please pop over to Apple Podcast and leave a review for the Model Health Show. And on that note, let's get to our special guest and topic of the day.
Dr. Tom Walters is a board certified orthopedic physical therapist and strength conditioning specialist based in Santa Barbara, California. In addition to his clinical practice, he runs one of the world's largest social media accounts dedicated to physical therapy, pain relief, and mobilization. He's @rehabscience on Instagram.
Dr. Walters has a Bachelor of Science degree in Exercise Science and a Doctorate in Physical Therapy. And he's been practicing physical therapy for over 17 years. From 2012 to 2019, he served as a full-time kinesiology professor at Westmont College and taught courses including biomechanics, therapeutic exercise, and pain science.
And now he's here to share some of his incredible insights, tips, tools, and strategies. Let's dive in this conversation with the amazing Dr. Tom Walters. Dr. Tom Walters. Good to see you, man. Thank you for coming and hanging out with us.
DR. TOM WALTERS: Thanks so much for having me. This is awesome. Thank you.
SHAWN STEVENSON: Of course, of course. So, let's start off by talking about the science of pain. What is pain exactly?
DR. TOM WALTERS: Yeah, no, this is awesome. This is such a huge, it was a huge focus of the book and something I really wanted to include. There's good pain science books out there for clinicians, but there's not a lot of great information, kind of small little books out there for the general kind of regular population.
And we have so much research from different studies showing just how helpful pain education can be. You know, there's so much fear and anxiety around pain when you're injured. We were talking about that before. You know, you just don't know like, what's going on? Is this serious?
Most people associate pain with some physical injury in their body and a lot of times we know that's not the case. So, there's a lot about pain education that can help reduce fear and anxiety and just get people moving in the right direction, so they don't become so fearful that they stop moving and suffer all those other deconditioning, atrophy, all those things that happen when you are sedentary and increase your risk of injury later.
So, when you look at the definition of pain, kind of the main body out there is the International Association for the Study of Pain. And the definition for pain nowadays is basically a physical or emotional, an unpleasant physical or emotional experience that they say is associated with actual or potential tissue damage.
And I think that part, "actual or potential tissue damage" is really important. And that's a, it's a recent change probably in the last 15 years. But most people again will think, "If I have pain, I have actual tissue damage." That something, "I've torn a muscle, or I've torn a ligament, or I've torn my meniscus. I've done something like that."
And really, we have a lot of cool studies showing that your brain, we know pain comes from the brain now from these studies, but it's this experience outputted by the brain in response to perceived threat or danger. So, we see situations where people will actually have pain when there's no tissue damage, but they believe there's the potential for it. And when you can make people believe there's the potential for tissue damage, you can create pain.
So, there's kind of crazy studies, a lot of them are of Australia. One of the most known pain neuroscientists is located in Australia, and he does a lot of study on this. So, it's a fascinating area. Just the brain in general is fascinating and pain is no different.
SHAWN STEVENSON: Yeah. You know, and I love how you kick the book off by deconstructing how we were programmed about pain recently in medicine, which is René Descartes and this kind of Cartesian model of very, looking at the human body is very mechanistic. Right? So essentially if you could actually just share what does that mean? What were we looking at pain as prior to this kind of new revolution that's taking place?
DR. TOM WALTERS: Yeah. So basically, and actually still a lot of practitioners function this way, which is unfortunate, but pain was looked at in this sort of linear relationship. It was called the Cartesian model, which is basically you would have something, basically pain came from the tissues of the body.
And it would just, so you slammed your finger, or you burned your hand or something and basically the thought was, oh, you've got these pain sensors or receptors in your tissue that relay that pain message up to your spinal cord, up to your brain, and then tell your brain, "Hey, there's pain down here. You got to do something about it." And really the more recent research on it has shown that we, it's more appropriate to think about it as danger receptors. We call them nociceptors. So, they're these small nerve endings in the nervous system that basically detect high threshold stimuli.
So, if you think about like if you were squeezing your finger, if you slowly increase the pressure in the beginning, it's just pressure, right? But at a certain point you can activate those nociceptors, those high threshold receptors, those sensors, and they will then relay a danger message. So that's nociception, it literally stands for "danger reception". And so that nociceptive message will travel to different regions of your brain, and then your brain basically decides, is it, "Should I create pain?"
And that's looking at everything in the environment, your brain is constantly weighing the situation. Because there are times where it's good to output pain when you have nociception, right? To, 'cause pain at the end of the day is about survival and protecting you and keeping you alive. So, there are times obviously when nociception is coming in, you've got these danger messages coming into the nervous system into the brain, and you want to output pain to protect the organism. But then there are times where outputting pain could actually be harmful.
So, one of the examples that's given quite a bit for this is if you're crossing a busy street and you twist your ankle, if you're out in that lane, having pain in that moment is not ideal because you're going to change how you move, you're going to slow down. You risk being hit by a car or a bus or something. And so, your brain has ways of blocking nociception. You can even, almost like a dimmer switch, you can turn it down and basically blunt that response so that pain isn't created so that you can get out of that situation and be safe.
And we see this all kinds of things like athletes, soldiers, there's all kinds of stories of really traumatic physical insults where the person experienced no pain. And maybe later they felt pain when they were safe, but not in that moment.
SHAWN STEVENSON: You gave the example of this guy having a bullet in his neck.
DR. TOM WALTERS: Totally.
SHAWN STEVENSON: And then he's showing up on a scan later, he's like, "Oh, there's a bullet in there I guess."
DR. TOM WALTERS: It's crazy. Yeah. That there's all kinds of ones like that where people have had these traumatic things. I mean that guy, yeah. Bullet in the neck, goes in for some other issue. And they're doing a scan on his neck and discover there's a bullet in his neck. And for whatever reason, his nervous system just didn't think of it as threatening. So, he never experienced pain with it. So, it's, pain's a, it's a super interesting experience. It varies. Obviously, we all vary in terms of our pain perception and threshold.
And I talk about it, they talk about it in the pain neuroscience world is they call them neural signatures, these patterns of areas of the brain that fire when creating pain. It's almost like a fingerprint, it's a lot of the same areas, but people are different. You know, if you take people with back pain, lower back pain, even if their symptoms are somewhat similar, if you look at their brains, the pattern of neurons that fire to create their individual pain is different in each person.
SHAWN STEVENSON: Yeah. That's also fascinating too, is that no two people experience pain the same way. In the history of humanity all of us have a unique kind of signature, like you said, they're our fingerprint when it comes to pain. And it's based on obviously we've got these sensors in the cell. We're going to talk about that in a moment. Our brain and nervous system.
But also, our perception of things and also stress levels, various stress inputs that you talk about. And just to unpack this a little bit more, I want to talk about, you also highlight something really important in the book that pain is valuable. We see pain as just bad. We just want to get away from all pain, pain is bad. But pain is a really valuable kind of educator in our system.
DR. TOM WALTERS: For sure. Pain is a great teacher. I think when the nervous system, it can get tricky when people have chronic pain. And even in those situations, a lot of times it still is a teacher, and it can help you, help inform. If you can be aware and try to really cue in on all these factors that can influence pain, not just the physical body, but your thoughts and beliefs and stress and sleep hygiene and nutrition, and all of these things that can influence your nervous system and can sensitize it.
There's so many of those factors that people aren't aware, and I think when you learn about those, this is where pain education can become important. When you learn about those, you become aware of them and you can start looking at what is, why is this pain occurring and what is it telling me about my life. You know? And so, most people will only think about pain as, "What's wrong with my knee? You know, what's wrong? Is my, do I have arthritis? Do I have a meniscus tear?" They will try to blame all pain on something in the physical body.
And for sure there are situations of pain that are very much associated with the biological system in your body, but lots of people have pain. I have a pain issue in the right side, kind of, of my thoracic spine that started six years ago pretty much at this point that started from a physical injury. I was in jiu-jitsu, and I hurt a rib. And it was at a time period in life that was stressful. I was in a stressful job. There was just a lot going on. My kids were young. Just, I was kind of ramped up.
And to this day, that tissue is healed, right? There's no injury back there anymore. But if I get stressed out, particularly that seems to be the trigger. Even if it's positive stress, like I'm about to go on vacation, that spot will start hurting. So, we know from the research that our endocrine system, different neurotransmitters in the nervous system, when those things are in bloodstream, cortisol, elevated cortisol levels with stress, those things can sensitize your nervous system.
And so it's really important to be aware of all these factors that influence pain, and again, can be a really powerful teacher if you can really try to focus in on it and think about it, a lot of times it can help you identify these things that might be off in your life, usually that pain is trying to tell you something.
You know, something is not right, almost like a balance. There's something maybe out of balance in your life. And I think for a lot of people that... And in a lot of cases, if pain persists is related to stress, poor sleep, and nutrition factors. And probably a lack of exercise and just general movement too.
SHAWN STEVENSON: Wow. Again, just looking at historically or in our modern culture, seeing pain as something mechanistic where a tissue injury is informing your brain that there's a problem here, in reality, however, our brain is deciding all of these things, is deciding how much pain, whether to even express pain, and it's based on our perception, whether it's kind of very conscious or deeply unconscious as well.
And this is highlighted in, you shared a couple of studies, and you talked about phantom limb pain, for example, like you shared in the book, 85% of people who've lost a limb experienced pain in that limb that no longer exists. And you also shared this study, if you could actually share it now, it involved the metal rod and different colors. Talk about that?
DR. TOM WALTERS: Yeah, it's a great study. It's again, from Lorimer Moseley, this pain neuroscientist in Australia. And they did this really cool study where they took people, healthy people who didn't have pain, asymptomatic individuals and brought them into the lab and basically would show them different colors. And in some cases, they'd also let them look at their own hand.
And then they would touch them with a rod, a metal rod. And the metal rod, they're touch them on the back of the hand. The metal rod is always the same temperature. But what was interesting, and then they'd ask people to rate how uncomfortable the stimuli was, and if people saw... The two colors of lights were red and blue. So, if they saw a red light, they would report that it was more uncomfortable than if they saw a blue light.
And this relates, a lot of pain is related to meaning, what something means to us. And so, color has this meaning of temperature, those two colors. And then also if they were allowed to look at their hand when it was being touched, they would report more... Being more uncomfortable. And this is why I tell kids not to look at getting a shot, because if you watch that needle be inserted, it will usually be more uncomfortable for people.
So just a cool study where you're basically creating pain and an uncomfortable sensation in people who have none of that at the start of the study, just based on the meaning of something. And the phantom limb pain is where all this kind of started. These studies, again, people who have lost a limb, you having an amputee, maybe a soldier who loses their leg below the knee, have a below the knee amputation and still have pain in their foot. And so, it's this, again, it goes back to how influential the brain is and how important the brain is.
Obviously, you can't... Thinking back to the old Cartesian model, you don't have any stimuli coming from that foot, it's not there anymore. But when we look at the brain, you have this thing called a homunculus, which is basically a motor and sensory map of your physical body. Your physical body is, obviously you have your physical body, but you also have a map of that physical body in your somatosensory cortex.
And so, the brain in those situation seems to be still thinking there's some danger down here, maybe because of how traumatic the incident was when it happened, so I'm going to keep outputting pain. Then like those studies show, up to 85% in those people that have lost their limbs.
SHAWN STEVENSON: It's no longer anecdotal at that point.
DR. TOM WALTERS: Yeah.
SHAWN STEVENSON: That's really remarkable. And again, it's just demonstrating again that the brain is first really in this decision. And also, this really speaks to with pain management, how important it is to manage our minds.
And it reminded me when I read this study, there was a study conducted by Alia Crum and some other researchers, her team at Stanford at the time, and they get a skin prick test. And this was a histamine test where they would create a rash basically for test subjects and within six minutes, they would develop a rash.
Now they have a physician to apply a cream and the cream is completely inert, but some of the test subjects are told that this cream is an antihistamine cream, it's going to make your rascal away. Other people were told that this cream is an agonist, is a inflammatory agonist, it's going to make your rash worse.
Across the board, everybody's rash got better or worse based on the message they received, and the biggest determinant on how much the rest changed, either went away or improved, and this happened all within 10 minutes after them applying this cream. Again, there's no therapeutic ingredients in the cream. Was based on, again, how quickly it changed and how much a change was based on their perception of how competent they believe the physician was. Right?
So how much they believed in them determined how much this rash changed. And again, it was a placebo cream. So, this again speaks to the power of our minds and what we believe and how we associate with things based on our experience, based on our stress at the time, as you showed, talked about already and you demonstrate through the book.
And I love that because this isn't talked about in regards to pain, could your pain be exacerbated or caused or continued and not resolving because you're sleep-deprived, because you're making your tissues out of low quality things or you have a poor diet? Or like you said, you're experiencing stress, whether positive or negative?
DR. TOM WALTERS: Yeah, yeah, for sure. No, those things, that whole placebo and nocebo is the opposite. This is a huge area that I have been interested in for years, just the idea that you can have harmful experiences and things happen in our body based on messaging and what you believe.
And a lot of people don't know about the nocebo, but basically the opposite of the placebo in that study you mentioned. There's lots of studies out there like that, where they show that you can totally change someone's... Even pills are like this, pills that are different shapes or pills that are solid in color versus translucent have different effects.
SHAWN STEVENSON: The size of the pill.
DR. TOM WALTERS: The size of the pill. Yeah, so people have beliefs about those things and that will change how they respond, how their physical body responds. And you have it both directions, like you said, the practitioner thing is huge, there's acupuncture studies where they've shown that people respond better to acupuncture if they have a clinician that is Asian.
And I think even if the practitioner is an older male, people tend to believe that that's going to be a more experienced sort of credible acupuncturist versus if you have a Caucasian female doing the acupuncture.
SHAWN STEVENSON: Who's very young.
DR. TOM WALTERS: Yeah, totally. People think, "Oh this person's not as confident or might not know as much about this." So, it really is interesting. Even in the physical therapy world, in my world, if a practitioner takes too long in their examination, people will start to lose confidence and outcomes in the session will become weakened by that, just based on that person's perception of how competent that practitioner is.
So, it's a huge... It's one of the most fascinating areas to me, again, that nocebo. 'Cause people just don't really hear about it. This is really why I got started doing a lot of stuff I did, was you would... I would constantly have patients come in who had had these harmful messages passed on to them from practitioners, and it was really frustrating. And sometimes it was done unintentionally, sometimes it was intentionally to keep them coming back.
But basically, people have all heard these stories, you go to a practitioner and it's like, "Oh, your back is out of alignment, you've got to come here for 60 visits to... " And people will be, these narratives will be passed on to people, that, we call them "thought viruses" in the rehab world and the pain world, that you're basically passing this thought virus onto them and convincing them that something harmful will happen to them if they don't follow this kind of plan of care.
And that's stuff's just frustrating 'cause so much of it has been debunked and doesn't fit with current, our current understanding of pain science.
SHAWN STEVENSON: Yeah. That's why I got into this field. Well, I didn't necessarily choose it consciously at the time, but I was 20 years old and got diagnosed with degenerative disc disease, and I was just a kid still, and the position told me that, "You'll never be able to walk normally again, you'll never be out of pain. This is something we're just going to have to manage. You're not going to get any better."
And these are some of the words that he would use essentially, when I'm just like, "Okay, so what do we need to do to fix this?" And he put his hand on my shoulder, he's just like, "I'm sorry, son, there's nothing you could do about this." I mean, man.
And I went from I went in because I was having a nuisance of a pain in my hamstring and not being able to extend my leg, and I went from that, and I've been dealing with that for maybe two months, and I went from that within a number of weeks to chronic debilitating pain where I couldn't get up without a lightning bolt of sciatic pain going down my leg.
And of course, to have a resolution, complete resolution of that and not only to get out of pain, which getting out of pain was a huge step. I had to deal with the fear then after when the pain was gone, of re-aggravating and being exceptionally cautious. But also... And I want to circle back and talk about that, but also having a, instead of a degeneration, a regeneration of those tissues. Things that are supposed to be...
We know that that's not the case now, but 20 plus years ago, this was just kind of the thing. And it's still unfortunately, some people, depending on the practitioner you see, they might tell you that you'll never walk again, you're going to be dealing with this forever, you got to be on this drug forever. And it's just, obviously it's irresponsible.
Not to say that they're trying to be negligent with the patient, they're just doing what they're taught and they're trying to help in the way that they're taught.
DR. TOM WALTERS: Yeah, there's a lot of false beliefs that still persist out there, and I think, like you said, I don't think most of those practitioners really are trying to hurt you or be harmful, they just literally believe. Unfortunately, the example you gave is a common one where too much weight is put on imaging, when people look at an X-ray or an MRI, a practitioner will look at it and make some prognosis based on a static image.
And like you said, we know that's totally not true now. There are so many people that have imaging studies that look really horrible and have no symptoms, this is done... There are lots of studies on this now, where they take asymptomatic pain-free people, put them through MRIS, and almost half of people have disc herniations, meniscus tears, labral tears in their hip and shoulder, arthritic changes.
And a lot of that stuff now is just... Again, this is where pain gets hard.
SHAWN STEVENSON: They have no idea.
DR. TOM WALTERS: They have no idea. Have no idea. So, a lot of times now we talk about that just being age-related changes, sort of like wrinkles, like your skin is changing. And imagine if we told everyone that, "Ooh, you've got wrinkles, I bet your face is really going to start hurting.?"
Right? So that's what's happening. You're looking at this and you have no real proof that this is pathological versus is it just an age-related change. And so, I always tell people, you've got to look at that stuff as a piece of the puzzle and having information is good if you can put it in its place.
So, imaging can be useful. A lot of times in rehab it doesn't actually change what you do, 'cause you're looking at symptoms and function and you just move forward in graded steps, but sometimes imaging is nice to have, and it gives you another piece of information. It's just important you put it in its place and don't over emphasize it.
SHAWN STEVENSON: Oh, and it's so powerful. Thank you for sharing that. Because again, sometimes we find a thing, it was just like, "This is the thing," and we become obsessed with that, and it can exacerbate our belief that we're broken. And in most of the cases, as you demonstrate in the book, it's far from the case most of the time.
And what that said, you also talked about... And just to summarize what we've already covered a little bit, but the brain essentially receives stimuli and decides whether those stimuli warrant a pain response. Your brain decides. But you unpack the biopsychosocial model for treating pain, let's talk about that?
DR. TOM WALTERS: Yeah, a huge one. Thanks for bring that up. That's kind of what replaced... So even when I went to physical therapy school, it was, I was taught basically the postural structural biomechanical model. So, we would have people come in with pain, pain's the number one symptom that really people go to seek medical care. And people come into physical therapy and the goal was, "Let's identify what tissue is causing this pain."
And so unfortunately, that's why most people want to blame their pain on a tissue. People want to get an X-ray and MRI, 'cause they want to figure out what's causing this pain. It's natural, you can understand that, but that was sort of... That motivation I think was really created by the medical system.
And so, then what we saw is that there's people who come in who have pain, and I saw this a lot of times as a new clinician that come in with pain and the postural structural biomechanical very physical tissue explanations wouldn't get some people better. And so, you have lot's of people who would get better, but you have some people who wouldn't. And that, for me at least, would kind of get me thinking like, "What's going on here? This seems there's something more complex or complicated."
And the biopsychosocial model, you look at "bio", which is the bio part of that model kind of encompasses all of that old posture structure biomechanic steps, all the anatomy, posture, force on the system, all the really heavy tissue things. And then "psychosocial" is just like it sounds. "Psycho" is thoughts and beliefs, mental health, stress. And then the social aspect is looking at people's social connectedness. We see research now that people with chronic pain tend to be more isolated socially, they laugh less. There's things...
That's even some of the recommendations for people with chronic pain is just to get a joke book or just watching a comedy special. Do something that makes you laugh because that can change... Again, you're looking at pain is associated with the nervous system thinking that it's threatened, and so if you can remove some threat in different ways, you can help to ramp down that sensitivity of the nervous system.
And so now we look at all of these factors related to that biopsychosocial model, and like you were talking about earlier, the mind is so huge in that. Your thoughts and beliefs, placebo, nocebo, what something means to you, the cultural background you have. Culture is a huge influence on what people believe about pain, whether or not they seek care, if it's a sign of weakness. There's kind of all these things.
You know, pain carries a lot of meaning with it, and so that model, and even that model now is starting to... There are other models coming in that may replace it. But I still think it's one of the best for considering the whole person. I think more and more practitioners really are getting better at thinking about that whole person.
SHAWN STEVENSON: Right, right. Because that's the thing too, is... And also, when you talked earlier about having our own unique pain signature, it's going to entail you paying attention to the person, the whole person.
DR. TOM WALTERS: And unfortunately, we have a medical model where the time isn't taken to be able to do that in the first place, so a lot of blanket treatments are done. And that's really what I was exposed to, which is you have this symptom cluster, here's this medication, and here's this recommendation to basically again become immobilized. Don't do anything. Bed rest.
SHAWN STEVENSON: They actually gave me bed rest. I walked in there, I walked in. I walked into the office, and he gave me a bed rest for two weeks. Are you kidding me? And again, just to wonder why I had an onset of more severe symptoms, because not only was I experiencing damage to that area of my spine, but now everything's going to start to atrophy. And so, can you talk a little bit about that where... And again, there's a place for all of these things, to immobilize. Again, if you have a leg injury, for example, there are... If it's extremely severe.
But the majority of the time... And you talk about this in the book too. You break it down like grade one, grade two, grade three. If you have a grade one injury and you go in, which I've experienced, and the physician want to put you in a boot. And you again, you walked in and they're saying, for example, this was my experience, that you wear this boot, this huge robotic leg thing for the next four to six weeks, come back in.
And then I even asked him, I was like, "Well, then should I do physical therapy after that?" And this was a bad Achilles strain, but it wasn't torn. But he used ultrasound, whatever diagnostic thing and said, "Oh, I'm glad that you came in because this looks bad, it could have got worse." And I felt that, like it could have got worse. But it can also get better. And to go from that, versus consulting, thankfully, you have this network to consult with other skilled practitioners and ask, "Is this a good idea?"
And nine out of 10 people are saying, "No, do not mobilize, that is not appropriate. Actually, we need to look at some possible strengthening activities." Of course, let the inflammation go down, don't do the thing that's triggering pain so rapidly, which for me, it was just going downstairs, that was pretty much the thing that hurt. I could walk relatively normally.
So, then I started to do some eccentric training with the calf and I got... When those four weeks went by, I was already 100% is, not necessarily internally, but I could do all my normal stuff. I could lift, I was doing leg exercises. And it was as if for me experientially that nothing had happened. So, can you talk about that?
DR. TOM WALTERS: Yeah, no, that's... Yeah, I mean, there's grades of injuries and so you've got to think about most of these things where somebody be mobilized like that related to tendon and ligament injuries. Fractures of course too. A fracture is kind of a different beast, and if you have a fracture that needs to be immobilized, that's kind of maybe the one time you'd really think like, "This is probably necessary depending on how severe or complicated that fracture is."
But man, when you get into soft tissue injuries, this was actually just published in the British Journal of Sports Medicine, but now we look at this, it used to be RICE, if you ever hear RICE, Rest, Ice, Compression, Elevation. That's kind of changed over time. And so, when you look at the new research on soft tissue injuries, which would be tendons and ligaments, most things in the physical body, none of that is immobilized. Actually, it's movement, you want to be mobilizing and moving the area. And of course, that's respecting your symptoms and your function at the same time.
But just like your example, if somebody walks in and can complete many functional tasks without symptoms and they don't show some other signs, like maybe it's what happens so much an ankle, or maybe somebody tore their ACL, maybe they have severe knee instability. And so, they, maybe not pain, but they can't control their joint, and the risk of injuring other structures like the meniscus or other ligaments, maybe there's a place for partially immobilizing them. Rarely is it full immobilization like the boot you're talking about.
But if somebody comes in, they're going to do some of those tasks without symptoms? No way. It doesn't make any sense to fully immobilize them. And it really should be more... Because again, you do that and you for sure are going to cause disuse atrophy, everything is going to decondition. And then to tell the person that they can just wear that and then go back to normal life is hugely irresponsible because now they are de-conditioned, the soft tissue injury risk is way higher because our body does not waste energy maintaining muscle mass and tendon thickness, ligament thickness, things like that when it doesn't need to spend that energy.
So, you are going to atrophy and that tissue is going to weaken, the capacity of that tissue will drop. And so, if you come out of being immobilized and just, "I'm going to go play basketball." Well, now your risk of rupturing your Achilles is way higher. So, we talk about this a lot with physical tissues, kind of the capacity of that physical tissue. You have to... That's a good way to think about it for people, is that our musculoskeletal system is extremely robust and adaptable, and a lot of times when people are in pain, they start thinking that they're fragile, they're going to break, something is going to happen.
And so, a lot of it is trying to reassure people, really physical therapy is mostly therapy, and the longer I've been in it, a huge part of it for pain is really therapy. And it's really trying to reassure people that the musculoskeletal system can adapt and change when you expose it to the right levels of stress. And yes, sometimes there is a place for being immobilized and letting something heal but being immobilized means that there's absolutely very minimal stress on the system and you're not going to help encourage an increase in that capacity of those tissues.
So, if you don't have horrible symptoms, you don't have a bunch of pain, you're not showing other signs that if they were present could lead to other injuries of other structures, then yeah, of course, you really want to keep moving in the ways that you can, and then with gradual increases in stress, build up the capacity of that tissue. And that's usually mostly resistance training. Resistance training has by far the most evidence, and that's mostly mobility, things like that have a place of course, early in rehab, but most of it is on strengthening, like you want to strengthen tissue, and if you're immobilized, it's for sure getting weaker.
SHAWN STEVENSON: In the book here, Chapter 2, which I've got this beautiful book here for folks that are watching on the video version, you need to pick up a copy like ASAP, you say, this is a direct quote in the book, "Research shows that people who understand how their nerves function are less fearful and feel less threatened by pain, which can help reduce their symptoms." So, it's an education about their bodies, what's going on in your own body and having the authority, having the agency to manage.
Again, when you have the responsibility of healing an injury, rather than immobilizing a tissue, you need to be able to know your threshold and pay attention to your body, like, "What can I do to help to push this healing process forward without going too far?" Because it's not going to be exactly cookie cutter what prescriptive thing is going to come from a practitioner.
And also, let's just be honest, this is part of the reason I wanted you here. There's a lot of disrespect of the physical therapy field. Alright? Because if I'm going to... If I'm in pain and I'm going typically to a surgeon, right? Again, even with the Achilles thing, they're a surgeon, surgery and drugs is the main two things. Of course, they might have people who they outsource to as far as PT.
But this particular fellow, as well meaning as he was, he was just like... I asked, "Physical therapy after this?" He was like, "No, you should be fine to just kind of work your way back into normal activity." And it's so inappropriate because your field is one of the most valuable. And you said it before, I was going to say this before you even said it, the therapy part of it, that's what's overlooked. Because it's not just the psychological aspect, but you have therapy through movement too. It's a powerful combination.
DR. TOM WALTERS: Yeah, it's huge, I think. I really think of myself more now as a coach for people, because people have to have the mindset that getting better from pain injury requires active participation in most cases. You have to as the individual take responsibility for your body and actively participate.
Too many people think of it as just this passive thing, "I'll go get a... I'll go see the doctor and they'll give me some medication. I'll go to the chiropractor; they'll adjust me and that'll fix it. I'll get a massage and that will fix it." And while there is a place for a lot of those things temporarily, by far the research shows that these active things like education, movement and exercise have way better evidence in the long term for not only rehabilitation, but the pre-hab idea of helping to prevent injuries.
I don't want to say prevent, 'cause that's never 10%. We all get injured. It's reducing the risk of suffering an injury. And so that component is so important to people to understand. And I think when you understand more about the science of pain and injury, well, not only are you less fearful when you do have those things come up, less anxious about what it means, you can kind of... I know for me, having this background, when I have pain or an injury, most things we get are more just kind of like irritations. It doesn't mean something was really torn or damaged. In most cases.
And so, when you know that and you have that mindset and you have a plan, anything in life that is unknown is scary. And so that's totally true of pain when you don't fully understand it, you're more likely to be scared of it and threatened and feel anxious and fearful, and those things have been shown to actually make pain worse in a lot cases.
People will become more hyper-vigilant, they'll stress about it, and we see that when people move from an acute pain state to a conic pain state, there's usually those kinds of factors where their stress, anxiety, hyper-vigilance, fear, and those things wind up the nervous system and make it more sensitive. So, understanding pain and injury helps reduce some of those thoughts and emotions, and it gives you a path for.
And I think because there's so much evidence for active things like movement, exercise, of course there's lots of other factors that we talk about in the book you want to think about, but because there's so much evidence for those, you can do those on your own, and if you are willing to take responsibility, you can pick up something like a book that has programs that, aren't obviously aren't tailored to you specifically, it's not like I did an evaluation and gave you this program.
But if you know how to modify based on paying attention to your symptoms, guidelines that are outlined in the book, you can take the programs, create programs for yourself and basically make your body more resilient, get past pain and injury on your own, and I think that's a huge thing for people.
Again, it's okay to go see a practitioner. Of course, you're not getting better, go see someone. If you want to implement some of these passive interventions temporarily. I still do manual therapy on people; I will work on them to do things as kind of a jump start to getting rid of pain. But the message at the end of the day should be, there's a ton of things that you can do on yourself, and those have the best evidence in the long run anyways.
SHAWN STEVENSON: Man. Got a quick break coming up, we'll be right back. I've got some very bad news for you about vitamin C supplements. Most people have no idea that typical vitamin C supplements are made from corn syrup or corn starch derived from GMO crops. The synthetic ascorbic acid found in most vitamin C supplements is structurally similar to naturally derived whole food sources of vitamin C, but they are not the same thing.
Whole food and whole food concentrates of vitamin C have hundreds of other bio-active co-factors that make vitamin C work miraculously in our bodies, while synthetic vitamin C is the very definition of a one-trick pony. In fact, by be devoid of essential cofactors, synthetic vitamin C supplements can be outright harmful to your health.
For instance, a 2013 study published in the Journal of the American Medical Association, Internal Medicine, found that participants taking synthetic vitamin C supplements had twice the risk of developing kidney stones. Another study from researchers at USC on a daily dose of synthetic vitamin C thickened the walls of participants' arteries two and a half times faster than those not taking a synthetic supplement.
This is absolutely insane because, number one, it's one of the most popular standalone supplements in the world and commonly found in most multi-vitamins. Number two, whole food-based whole food concentrates of real vitamin C are remarkably effective in lowering the risk of cardiovascular disease, even in people engaged in high-risk behaviors like smoking.
A randomized placebo-controlled study published in the Journal of Cardiology had 20 smokers consume a whole food concentrated vitamin C in the form of camu camu berry daily over the course of a one-week study, and it led to significantly lowered oxidative stress and lowered inflammatory biomarkers. What's more, there were no changes in these markers in the placebo group who received an ordinary synthetic vitamin C supplement.
Because of the damage humans have done to the soil microbiome, levels of Vitamin C are notably lower in typical foods. That's why I've been utilizing a whole food vitamin C concentrate blend of camu camu berry, acerola cherry, and amla berry for years, and I'm on a mission to spread awareness about this and get people off synthetic vitamin C supplements.
The Essential C Complex from Paleovalley is all organic, no synthetic ingredients and no fillers. Plus, it has a 60-day 100% money back guarantee. So, if you aren't absolutely thrilled with it, you'll receive a full refund, no questions asked. Go to paleovalley.com/model right now, and you automatically receive 15% off of your order at checkout.
Vitamin C is critical for our immune system health, but also the health of our heart, our brain, our skin, and so much more. Target organic whole food sources of vitamin C. And you're going to supplement, make sure it's a whole food concentrate and not synthetic vitamin C. Go to paleovalley.com/model, that's P-A-L-E-O-V-A-L-L-E-Y.com/model right now for 15% off, and now back to the show.
I want to dive a little bit deeper into the fact that we have sensors in our bodies. We think about maybe the, Jennifer Lopez has a new movie, it's called The Mother, and she's like an assassin but she's also a mother, but she's got set up around her property, these different sensors and even some landmines, for example, to protect the premises. But we think about that in terms of technology, but we have an ultimate technology in our body. So, can you talk a little bit about these sensors in ourselves?
DR. TOM WALTERS: For sure. Yeah. No, the nervous system is amazing. I love him to think about it like the sensors on your car dashboard, and talk about that in the book, an oil temperature light, your tire pressure gauge, there's all these things that could come on to alert you to potential problems with your vehicle, and so your body has similar types of things.
So, we've got temperature sensors, chemical sensors, pressure sensors, there are immune system sensors, blood flow sensors. So, these things, again, are kind of there in a lot of cases to... I mean, lots of different functions, but in a lot of cases to protect you, and so to identify a danger. You think about something like the immune sensors are actually kind of interesting, a lot of people will say, actually, if you talk to people who have had bouts with different pain issues, low back pain is a good one, neck pain is a good one, when they... Sometimes people say, when they get sick, their pain comes back again.
And so, a lot of that is thought to immune system molecules that are present in the bloodstream, some of them can actually activate your nervous system and turn on, activate those nociceptors, those danger receptors. So, you'll hear people say, "You know, all my low back pain came back when I was sick," and in a lot of those cases, not because they suddenly re-injured their low back or activated that pain issue. It's those fibers being sensitized by the immune system.
Sometimes you'll get people who say that their pain comes on with different changes in temperature, barometric pressure, things like that. So yeah, there's all these kind of interesting sensors with crazy names or pressure sensors, we've got Meissner's corpuscles and Pacinian corpuscles, there's all these kind of crazy names for these different sensors. But yeah, the nervous system is fascinating, and I think... I always... I had the opportunity several times in my education to dissect humans, and it's really pretty cool to look at our nerves.
I think people generally have kind of a good... They can visualize a muscle and even tendon and... I'm not going to talk about fascia, since so many people have an idea of what fascia looks like. But a lot of people don't know how big their nerves are, and so you look at something like the sciatic nerve, it's like the diameter of a pencil. The nerve that goes to our carpal tunnel. All these nerves look like kind of like spaghetti noodles. And I think when people just...
We see this in the research over and over again, that when people understand their nerves, they're less scary and then pain is usually less scary, and that usually helps the pain experience, it helps the nerve system kind of calm down. So, the nervous system is super interesting.
SHAWN STEVENSON: Yeah. That was a big light bulb moment reading the book, when you mentioned how folks get a cold or flu and then they have back pain that activates, and you described how that can even happen. Even just now mentioning changes in weather, people like feeling pain or stiffness based on changes of the weather.
And again, having that association, we have sensors that are monitoring pressure, that are monitoring temperature, and all of these things are really... There's a memory involved, cellular memory, but they're all intertwined and communicating, your brain is putting all these pieces together. So, you mentioned that we have these sensors for temperature, movement. Of course, we think again, the movement is a thing that causes the injuries.
DR. TOM WALTERS: How do I not mention that one?
SHAWN STEVENSON: Pressure, stress, immunity and blood flow as well. So again, there's a intricate connection with the nervous system and these various sensors, and a stressful time can kind of reactivate an old injury or something. But this also points of something I don't think we think about a lot, which is what's healing an injury is your immune system. Immune system we think about in this very vanilla thing, like if you get a cold.
DR. TOM WALTERS: Totally.
SHAWN STEVENSON: So, let's talk about, again just to re-emphasize, essentially, your nervous system can dial up the sensitivity of these sensors or it can dial it back down. And this is one of the biggest revelations in your book, because when we talk about things like neuroplasticity, we just think about the sunny positive side of it, we don't think about the fact that we can create neuroplasticity in ways that are negative in a sense, and degrade our form and function based off of an experience.
So now here's the thing, when we're experiencing pain, chronic pain, we've got this certain association going on in our bodies, and neuroplasticity has laid down all this information to make this constant, but we can use a positive neuro association or neuroplasticity to reverse engineer the pain and get people out of it.
DR. TOM WALTERS: For sure. Yeah, this is such an important piece for anyone in pain to understand. Because it can go both directions, you can have positive and negative neuroplastic processes, and most people think about yeah, just the positive side, which is awesome that we have, that your brain can continue to develop, and you can grow new synapses and all these things that happen with exercise and movement.
But there's also the negative neuroplastic side, and your nervous system, when you think about pain, can change to make you more sensitive. Basically, it will decrease your pain perception threshold so that you... It takes a smaller stimulus to reactivate that pain experience. And so, you'll hear about people who have really sensitized nervous systems where they might just be brushed lightly on their arm, and that creates this excruciating pain, and so we talk about hyperalgesia, this kind of heightened response, and allodynia, these ideas that where people have pain to a normally non-painful stimulus. And that in chronic, even chronic or persistent pain is thought to be associated with a negative neuroplastic process.
So basically, the body is ramping up the sensitivity of those sensors and the nervous system overall, because it feels like there's continued danger and it needs to protect you, and so out-putting pain as the way to protect you.
SHAWN STEVENSON: So, like use the example, for example, of somebody getting... I said, "Use the example, for example." Of somebody who gets injured picking up something heavy and the tissues were healed, the injuries healed, but then they have repeated injuries from picking up something very light, maybe picking up a pencil of the ground?
DR. TOM WALTERS: Yeah, this is a great one. Low back is such a great one. You can even think about your story from before about imaging. So, say you go see a doctor, you've got back pain, you're told you have severe degenerative disc disease, and you see this image. And so already you're thinking, "My back is in trouble, I need to be careful. I need to be more... Just I need to be hyper-vigilant and pay attention to this so that I don't have this happen again or suffer some worse injury in my spinal cords there, like what's going to happen?"
And so, people, they get ramped up in that way, and then they have this fear and anxiety that's sort of... It's sort of like, it's telling the nervous system, "There is danger here, there's a threat and I need to protect myself." And so, then the nervous system can increase the sensitivity, say, in those movement sensors. So, then you go, you'll hear people, they bend over to pick up a sock, pick a pencil, their system is not loaded in a really stressful way, so there's not a lot of force, they're not dead lifting 150 pounds or something, they're just picking up a sock.
And they have this pain response that's completely over-blown and not a good representation of what's actually happening with their physical body. And that's sort of one of the primary definitions of chronic or persistent pain, is that you have this overblown response, the symptoms don't match up with the stimulus that the body was exposed to.
So that's one of the things we look at. We sort of look at these clusters. There's not really like a test for chronic pain, it's sort of looking at history and clusters of symptoms and just kind of what symptoms they have.
And back pain is such a great example of that, where someone might have had a physical injury in the beginning, maybe they were dead lifting or something like that, and were in the gym lifting. And maybe they were tired, maybe they hadn't slept as well. Maybe they had a little tweak a month or two back and they're getting back into things and whatever. All these factors come into play, and they injure their back.
And so, then they go see someone. Maybe they receive or they read stuff online, or they go on social media, and they find an account that unfortunately is putting out messages that are harmful in some way, and increase that threat, and then they become more fearful that the nervous system kind of winds up. And then any time they bend over, they have... And so, it's tricky because you can have very physical pains that just get re-aggravated, and so it is tricky sometimes to help people kind of figure out, "Do I have more of a chronic persistent pain disorder? Or do I just have this acute pain that I'm re-aggravating all the time?"
And so that's where we really start to look at kind of characteristics between true chronic pain and acute or mechanical pain, which is called nociceptive pain, which has more to do with those nociceptors. So, there's these different types of pain, you're kind of trying to help people sort their way through it. And the book talks a lot about that, Chapter 3 is all about the different types of pain and outline these characteristics so people can kind of understand more about what they have.
A lot of times you're doing all the same interventions, but your approach to them is different. So, when you were talking about neuroplasticity, for instance, if you have chronic pain, you're thinking a little bit less about, "I need to make this tissue stronger, more mobile." You're thinking... Instead, you're thinking more about, “How can I de-sensitize my nervous system?" And that is actually very similar to what psychologists would do for people with anxiety and depression and things like that, it's called graded exposure.
So, it's exposure therapy, so you are exposing the movement system to gradual doses of stress that... And you try to keep it below that flare-up line, we call it the "flare-up line". So, people, it's that point where if you hit it, you'll kind of reactivate your pain. And so, it's inevitable that that will happen.
I always say rehab is never this perfect linear, "I just get better." It's you're kind of all over the map. But you're looking for this general positive trend. And people will inevitably go past the flare-up line, your body is always kind of a trial-and-error kind of experiment, you're constantly testing things. But the key is to have that education, stay positive and keep exposing the system to small doses of stress and eventually it will adapt, and that's where neuroplasticity is positive when it comes to pain.
SHAWN STEVENSON: Ah. So good. We got to remember all of us that the healing process is not a straight line, so thank you for that. Because we tend to think again like, "Oh, I messed it up", or whatever, because of the fear. But there's no way that I could have progressed.
And you give a great actual exercise for people, you know, if somebody's having difficulty in bending over without inflicting pain or activating pain, even though there's no injured tissues, of just laying on the floor and lifting the knees and curling your knees up towards your body and holding that position. Same kind of physical action, but you're in more this kind of stable position in a sense for your brain and nervous system just to be like, "Okay, you're cool here."
Because that's literally what I started off doing. I was doing these very simple therapy exercises on the floor when I was 20 years old and got this diagnosis, but this was like two years later after getting some empowerment. And I couldn't have gone from where I was, where I couldn't even extend my leg without pain, to progressively... And each step along the way I had to, I couldn't have healed and got into this level of true health and wellness without addressing my mind and addressing the fear, because again, now tissues are healed, I got, I actually got a scan done after a couple of years later when I was out of pain.
And it helped me to like, "Oh okay, I must be better." Even though everything felt good, I felt functional. I was doing stuff that I hadn't been able to do. And I started off, I remember the first time that I dead lifted, and it was just the bar, and I was just aware, but also, I'm coming in like, "Man, I feel really good, I'm confident, I'm strong." I've been doing all these other things, but just not this one activity, right?
And so, I built a strong base, and so I did that. And then there's no way I could have progressed from that to doing four plates each side, eventually, you know, hitting 405, and that was just within a matter of years. And this just, again, speaks to not just rehabilitating the tissues, but addressing the mental component. And you do that so well in the book again and again and again. You actually... There's a particular thing that it's called, you said flexion sensitivity is the definition.
DR. TOM WALTERS: Yeah, flexion sensitivity is actually really common in the low back. A lot of people will notice this when their back is painful, that... And people can have extension sensitivity too, but we basically look at, are your symptoms triggered more by rounding your back, which would it be like bending over, sitting. Those are kind of the main ones that trigger people. But both of those put the lumbar spine into a rounded kind of a flex position, whereas extension would be arching your back.
And many people with low back pain will have a, we call it a directional preference. They'll have a preference in terms of, "One feels better than the other, and one triggers my symptoms." And flexion sensitive people are quite common, and like you mentioned that example in the book, you can take someone who has a flexion sensitivity, say, bending over and you just change the context of that movement, expose their movement sensors to that movement in a different context.
And so, one easy way to do that is to lay on your back and pull your knees up to your chest, and that's just one way of going about it, there's different ways to kind of grade that and progress it, but it's similar to like... I always give this example, if you're scared of snakes, I'm not just going to hand you a snake. That's not how treatment would work. Like you have something your anxious about. You might have someone first just think about snakes, and then maybe they have a picture of snakes, and then maybe they see a snake like at the zoo.
SHAWN STEVENSON: Maybe they watch Snakes on a Plane.
DR. TOM WALTERS: Exactly, totally.
SHAWN STEVENSON: Don't watch that.
DR. TOM WALTERS: But you know, you're looking at gradually exposing the person to that threatening thing. And so, with pain, with physical pain, of course, it's mostly involving the physical body, so you're tending to look at graded exposure concepts that involve the movement sensors and the movement system, but like you said, it's biopsychosocial, so therapy is everything.
Some people who have pain are more affected by their thoughts and emotions than anything in their physical body, and so graded exposure in those individuals is more about their thoughts and emotions to overcome physical pain than some movement thing. So, you see this with low back pain, it's another good example, where something like depression is more associated with lower back pain than almost any physical characteristic, hamstring link, core strength, like any of these things.
Mental health is hugely tied to low back symptoms, there are lots of people who report their back pain is worse when they're at work, than when they're doing the same... They could be sitting on their desk at work and have had back pain, and then they're sitting watching TV at home and they have no back pain.
It's the same stress pretty much to their physical body, but the change in environment and what that does to their psychology, it changes those other sensors and influences those other factors that we know are involved with pain.
SHAWN STEVENSON: Wow, wow. This speaks to, again, that neurosignature that you talked about earlier, and how no two people are experiencing or perceiving pain the same way. At all, like we are all different. And we have a unique kind of patchwork quilt of experiences and input, and we've got to really be empowered, and this is why a book like this is so important, because even working with a skilled practitioner, still you've got to do your inner work. It's not just working out; it's working in and paying attention to these things.
And I would love if you could talk about this because this is one of the things that gets confused in a lot of people's minds, but what is an injury as opposed to pain?
DR. TOM WALTERS: Yeah, it's a huge one, and we've kind of alluded this a little bit, but this is a huge thing for people to separate and we talk about this, have a whole chapter dedicated to just separating pain from injury. But pain is that unpleasant experience we were talking about, it's something that's outputted from the brain. You could have pain and not have an injury; you could have an injury and have no pain. There's lots of, pain does...
Pain is an experience, again with actual or potential tissue damage and heavily influenced by thoughts and emotions and all those other factors. Injury really is a little bit more simple, I think. It's what most people think of when they think of having pain. It's a physical insult to your body.
So, in the musculoskeletal system, they kind of break down into different tissues, so you have muscle injuries, tendon injuries, ligament injuries, cartilage injuries, bone injuries. Those are kind of the big ones that people are going to experience. And those... It's important to know about injury because if you do in fact have an injury, you want to know what tissue that is. Because tissues heal at different time frames, mostly according to how much, their blood flow. So that can help you just have realistic expectations in terms of how long this might take to heal so that I can get back to whatever things I like to do in life.
So, we were talking about this earlier, ligament injuries are a great one. ACL tears, right, like ACL tears, there's so much in coverage of ACL tears these days. And the ACL is a ligament and ligaments tend to take longer to heal and get back to full strength. And so, when we look at human studies, they've found out that in athletes who have ACL tears, if they return to sport prior to nine months, their risk of injury goes up quite a bit, their risk of re-tearing their ACL.
But if you get past that nine-month mark, of course, you have to pass a certain strength and functional tests, but if you pass those tests and just get past that timeframe, it will give that ligament time to remodel and heal and your risk of re-tearing that ligament goes way down. So, we want to think about pain and injury as being different things often associated, but if you have pain, you want to not automatically jump to thinking, "I have a physical injury in my body," 'cause you might not. And so, you want to first kind of think about, it doesn't necessarily mean that.
Of course, if you do have a pain issue and you had maybe a traumatic something happened, like you twist it or you were sprinting and something popped, some other sign or symptom and there was high force on your system. Or you were dead lifting heavier than you normally do. If there was high force on your system and you have pain, then yeah, you kind of want to rule out an injury.
But they are different things, so it's important in a lot of ways, kind of changes your mindset and your approach to how you go about those things. I think in a lot of ways with an injury, it sometimes means that you have to be a little more respectful of how long that tissue takes to heal. Because if you rush that, you risk making it worse, damaging it more severely, and ultimately that just impairing your function and slowing down your ability to get back to the things you want to do.
SHAWN STEVENSON: You just mentioned remodeling, you go through and share with everybody in the book the phases of healing, and there's inflammation, maturation, and remodeling. Can you walk us through those?
DR. TOM WALTERS: Yeah, so a lot of those kind of wound healing time ideas come from actually wounds on the skin and things, but our physical body goes through these three basic healing sorts of phases, and we use those to... Those were sort of the foundation for the phases in the programs in the book, so the programs have three phases that sort of line up with the phases of healing. And again, you have to kind of...
It's helpful to know what tissue you're talking about. 'Cause there's a huge range, right? And it's going to depend on the grade of the injury, if you just have a minor ligament, you just barely sprained your ankle and have a grade one sprain, that's going to heal faster than a grade three, where you've completely torn the ligament.
But you've got these phases, and so the inflammatory phase is kind of that huge immune system part, where your immune system is really active and coming in and kind of cleaning up damaged tissue, macrophages, all these things are coming in. This is actually why we've kind of moved away from ice after injury, soft tissue injuries. Ice isn't really recommended too much anymore. Sometimes with really advanced surgeries, it can be helpful.
But most soft tissue injuries, ice actually can slow the infiltration of macrophages, and so it looks like it might actually slow the healing process. You want some inflammation. So, we have that. And that's typically a few days to a week, depending on how severe it is. And that's the one time in pain and injury where you might have rest be a part of what you're actually doing. I always have them...
SHAWN STEVENSON: Made them partial to full immobilization.
DR. TOM WALTERS: Exactly. And by rest, it's more of like an active rest, rarely are people completely sedentary. You know, say you injured one ankle, you'd still like to be kind of moving that a little bit, maybe you're just doing some basic mobility kind of exercises, kind of ankle pump type things. You're still as much as you can, strengthening your upper body, your other leg, there's all these benefits of continuing to train those other areas. So rarely is it I'm 100% sedentary.
But unfortunately, sometimes people are told rest is the only prescription, and we know that's totally not appropriate. So sometimes there's a little place for rest during that inflammatory phase when things are really sensitized, and then you go into that kind of maturation period, and that is usually kind of... They'll say about three weeks.
But you're really starting to lay the early foundation of building connective tissue and muscle tissue and kind of just rebuilding the area. Then after that is re-modeling and remodeling is the one that can really vary based on the tissue, but you know, maybe you think about that, starting around that three to four-week mark and could be going for two years. So, there are some studies showing that ligaments will... You can find evidence of the ligaments really remodeling up to that one to two-year mark.
So, it's, those are kind of the basic phases of healing and again, kind of nice to have in the back of your mind as... Especially if you have an injury, like if you know you had a physical tissue injury. They kind of aren't as important if you have pain, but if you have a physical tissue injury, you know a tissue is partially torn or stretched or something, you can kind of think about those phases as you think about your rehab.
SHAWN STEVENSON: Yeah, and it's going to be catered to you as you outlined in the book. And you just shared something so great, which is, again, we've got this particular tissue damage, it's a ligament and this could be stretched out for a year, possibly longer. Or if it's a minor muscle strain or tear, when we get to that re-modeling phase, it could be six weeks.
So, it just, it depends on the tissue, and it depends on you and your unique neuro signature, and it's just such a great resource to have to really get ourselves educated, because stuff's going to happen in our lives. And so, this has been an amazing man, amazing. What else do you want people to know that you have in the book and what they can look forward to?
DR. TOM WALTERS: Well, I think kind of alluding to what you were just talking about, I think most people are going to come to this book for the programs. It covers the whole body, it covers the 50 most common orthopedic conditions that in my 17 years as a PT, I've been treating.
So, it's all the things we get, plantar fasciitis, tennis elbow, rotator cuff pain, low back pain, sciatica, like it's all these things that... I'm a PT and I've had lots of these things, so I'm not immune to it. So, most people will come to the book for those programs, and I think there's obviously a ton of value in that. It's a program you can just go ahead and start. It's sort of like something a physical therapist would give you.
Of course, you want to think about all these things we've talked about to kind of tailor it to yourself, you don't want to go into something blindly and blow past pain, and you want to think about what you have. And I think my hope is that, I think there's a lot of people that are going to skip the first 10 chapters, the science of pain and injury, but I hope that people will come back to that at least. Because it really does give you a mental, a mindset, a framework for approaching pain and injury as you go forward. Because you don't want to feel...
Again, nobody wants to feel scared or anxious about pain or injury, and if you kind of understand your physical body, you understand kinesiology, your movement system, it reduces that, like I said before, something that's unknown is usually more likely to create fear in us.
And so, I hope people will come back to those chapters, there's a ton of research. There's almost 500 research citations in here. So, any of this stuff, it's not like I'm just making it up, it's not anecdotal, it's all cited, all the reference list is in the back of the book for all the chapters. I also think the other part that's helpful for people to think about when they go through this is that, of course when you think about pain and injury, education, exercise, movement are really huge, those are kind of the areas you think about first.
There's of course all the other factors, sleep, nutrition, stress management, all those are covered in Chapters 4 and 9, the factors that influence pain and injury. Once you have laid the foundation, you're thinking about all those things that form the kind of pyramid, like the base of that pyramid of recovery and healing, the other chapter that I think will be useful to people is the complementary alternative medicine chapter, which is basically every other intervention that people ask about, cupping, taping, electrical stimulation, visual imagery, cross-transfer, like stem cell, PRP. It's all these things that...
Like we were talking about before, a lot of them are things I would try. Like if I had a resistant injury or pain issue that wasn't getting better, I might go and try. I've got a labral tear in my left hip. I've had it for over a decade. And I can still function with it, it's not that big a deal, but there is a part of me in the back of my mind that thinks I've got an orthopedic surgeon friend of mine, might go do stem cell or PRP at some point, and just see what happens.
Those things are in that chapter, and they're linked... They're laid out in sort of a hierarchy of evidence, so the ones that come first in the chapter have more evidence and then it kind of goes down. But we can talk about the, you know, if you have the financial means and the time and you want to try other interventions, of course, prioritize the programs, exercise movement, other things in the book, but you can add those things, cryo, sauna.
There's a lot of research for these other things that can help boost your recovery. And a lot of times, doing those things to make people feel more positive, 'cause they feel like, "I'm doing something to attack this." And even if it has little actual, maybe it doesn't have a lot of evidence to it, but the placebo maybe you get from it, or feeling like you're doing something, you can't forget about that.
Almost half of medical interventions are thought to be hugely placebo-based. A lot of what we do in physical therapy is probably placebo-based. People believe they go to see someone, they feel like the person's competent and it's going to help them, just that belief is going to change their pain. So, I think that's another big chapter for people to go to besides all the other science stuff.
SHAWN STEVENSON: Yeah. You are the placebo.
DR. TOM WALTERS: Yeah. Exactly.
SHAWN STEVENSON: Shoutout Joe Dispenza. Is just getting armed with practical things that we can do, but also understanding the role of the mind. And like you shared in the book here, and I read that little snippet earlier, that getting educated about your body, getting educated about your nervous system, has been found to deeply impact pain and reduce pain, and we cannot negate that. So, man, this has been awesome. Can you let people know where to pick up a copy of the book and where they can connect with you online?
DR. TOM WALTERS: I appreciate it. Yeah, so the book, Rehab Science, you can find it on Amazon, Barnes & Noble, all the major book retailers. There's a lot of people who follow my account who are located internationally, and so there are groups, Blackwell's in the UK, bookstores like that that can ship it internationally. And then online, I'm @rehabscience, basically everywhere. Instagram, YouTube, Facebook, and then rehabscience.com. So yeah.
SHAWN STEVENSON: Awesome. This has been amazing, man. Thank you so much for taking the time and putting your energy into creating something as epic as this, and I just can't wait to share this with everybody.
DR. TOM WALTERS: Thanks man, thanks so much for having me. I am so looking forward to this thing getting out there, and I think like everything we talked about, any opportunity to kind of put out this educational type of information, I know it will help people. We have the research behind it. I've seen it with people in practice who have pain. And so, thank you to you for the opportunity.
SHAWN STEVENSON: Of course, my pleasure. Dr. Tom Walters, everybody. This is such an important topic, because again, most people are not going to make it through this human experience without going through tremendous pain and/or injuries.
And so, getting educated about what's happening internally with our bodies, with our mind and how our mind plays into the healing process, and also how our mind can exacerbate or even create injuries is incredibly important and one of those tools for us to be armed with to deal with pain, to deal with injuries when they do take place. It's so important, this happens to virtually everybody, but we just don't talk about it.
And so, I was thinking about during this episode, something really jumped out to me. We have this saying in culture, "adding insult to injury". Adding insult to injury. So you get an injury and then you get an insult on top of that.
But the reverse is also true. We can have an insult that causes an injury. We can have an insult, we can have somebody say something to us, we can have a belief implanted. Right? We talked about the nocebo effect, this outside influence, this insult comes in and this can create an injury within our bodies, this can create the outer manifestation of pain, of damage, based on what we believe.
And so, having the inroads and starting to understand and associate more appropriately and effectively and have a kinship with the power of our minds is so important today more than ever. And also, of course, that neurosignature understanding and that no two people experience pain the same way, and starting to cater things to ourselves when we're talking about our recovery protocols, it's so important. Because nobody else is living in your body. Hopefully nobody else is living in your body, shoutout to Men In Black. Alright, hopefully you don't got an alien stowing away.
But the bottom line is, you are experiencing life through your body, through your mind, and it is a unique, valuable experience. And getting the tools to better associate with that and to manage your own experience is more important than ever. Please share this out with your friends and family on social media, tag me, I'm @shawnmodel, and tag Dr. Walters, he's @rehabscience. Shout him out, let him know what you thought about this episode. And of course, you can send this directly from the podcast app that you are listening on.
We've got some epic master classes and world class guests coming your way very very soon, so make sure to stay tuned. Take care, have an amazing day, and I'll talk with you soon.
And for more after the show, make sure to head over to the modelhealthshow.com. That's where you can find all of the show notes, you could find transcriptions, videos for each episode, and if you got a comment, you can leave me a comment there as well. And please make sure to head over to iTunes and leave us a rating to let everybody know that the show is awesome, and I appreciate that so much. And take care, I promise to keep giving you more powerful, empowering, great content to help you transform your life. Thanks for tuning in.
Maximize Your Energy
Get the Free Checklist: “5 Keys That Could Radically Improve Your Energy Levels and Quality of Life”
HEALTHY MEALS EVERYONE WILL LOVE
The Greatest Gift You Can Give Your Family is Health
When you gather your family around the table to share nutritious food, you’re not only spending quality time with them - you’re setting them up for success in all areas of their lives.
The Eat Smarter Family Cookbook is filled with 100 delicious recipes, plus the latest science to support the mental, physical and social health of your loved ones.











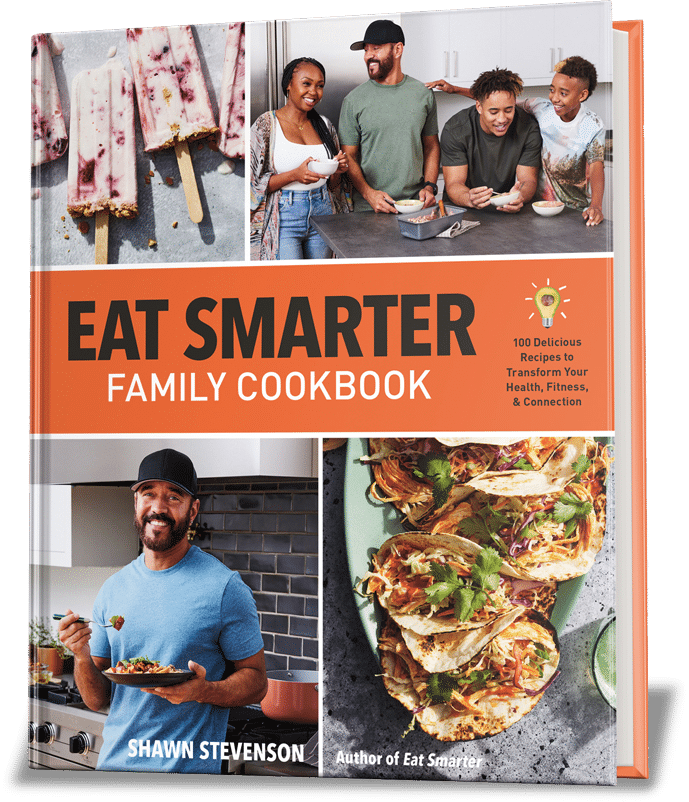
Share Your Voice
0 comments. Be the first to leave a comment.